You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Implant dentistry has provided predictable and reliable restoration of function and esthetics for patients plagued with tooth loss or regressing dental health requiring tooth extraction. The Brånemark research1,2 introduced to the dental profession the biologic foundation for evidence-based implant dentistry and revolutionized tooth replacement with dentistry’s ability to optimize function and esthetics with fixed implant-supported prostheses.
Immediate implant sites3-9 with and without immediate provisional restorations10-20 have been studied extensively in the literature. It is the purpose of this paper to report on outcome analytics comparing 26 years of documentation of immediate implant surgery and 13 years of documentation of immediate implant surgery with immediate provisional restoration.15-20
A complete, in-depth retrospective on this subject is forthcoming; this article is meant to be a summary of a subset of immediate implants, immediate implant/immediate provisional restoration (IIIPR), to give direction and present conclusions. This paper will discuss reliable IIIPR protocols that are evidence-based and provide expeditious transition from failing teeth to stable implant solutions that are functionally predictable and esthetically optimal.
Materials and Methods
Since February 1988, all implant procedures performed by the author were documented in a software module particular to implant dentistry (The Implant Tracker, www.implanttracker.com). This software became the repository of all the data for every implant site (n = 13,630) and it provided outcome analytics to compare success rates of varying protocols, including IIIPR (n = 2,056) and immediate implant/no restoration (IINR) (n = 5,284). The remaining implant sites were intact (n = 6,290) and were not included in this report.
The data files contain the date of surgery; pertinent medical and dental history; site of surgery; presence of infection; extraction information; size and type of implant placed; bone and soft tissue regenerative protocol and materials; site as a staged, immediate, and/or immediate load; date of integration confirmation; incidence of implant failure; and prosthetic completion and follow-up.
Intraoral photographs of the procedure showing the early healing and follow-up to completion and recall were also documented. This was intended to confirm esthetic harmony of the final prosthesis to the dentition and the congruence of the soft tissue result. Initial and periodic radiographs and photographs were taken to compare the bone and soft tissue landmarks years later under loading and long-term function.
The implants used varied in design and prosthetic connection. The IIIPR implants included rough-surface tapered implants with varying thread pitch and design; varying internal connections including trilobe, conical connection, and platform shift; and multiple prosthetic connections including both screw and cement retention. Bone graft material used universally was demineralized, freeze-dried bone allograft of 300 to 500 µm. Temporary prostheses for immediate restoration and final prostheses were either cement- or screw-retained with a single tooth or multiple teeth. In cases of cementation, a universal protocol was used to extrude cement extraorally on an analog of the final abutment prior to seating clinically to remove excess cement and minimize the introduction of subgingival cement. The majority of temporary restorations for immediate load were cement-retained and adjusted to be out of occlusion.
The implant software prompted the clinician to complete all the steps for each site for each patient from initial surgery and integration confirmation to prosthetic completion and patient recall evaluations.
Immediate implant exclusion criteria included the inability to stabilize the implant in the residual bone after extraction and debridement and exclusion criteria for immediate provisional restoration included the inability to attain implant stability greater than 30 Ncm. Insertion torque forces were visible on the electric drilling unit used and were titrated at implant placement so final seating could be accomplished to an insertion torque greater than 30 Ncm irrespective of the quality of the bone.
Surgical Protocol
One clinician completed all surgical procedures in a private practice setting, and multiple private practice dentists provided the final prosthesis in each case. Surgical protocols included primarily flapless surgery with atraumatic extraction with elevation from the mesiolingual, direct lingual, or distolingual to avoid altering labial soft tissue or papillae with full debridement of the sites down to sound bone. Root separation was performed prior to extraction of multi-rooted teeth, and in the presence of ankylosed roots, a radiograph was taken to confirm the absence of residual root. In the presence of a diminished labial or lingual plate, a bone graft was completed to reestablish socket contour with no flap elevation. If labial fenestration was present, a bone graft was placed from the socket side of the fenestration with no flap elevation and compression of the bone graft with the last drill used to establish the corridor for implant insertion.
Implants were placed precisely to conform at the restoration level to the esthetic and prosthetic needs of the site and at the apical level for stabilization in the very best available bone corridor. A high initial insertion torque was utilized, and the socket sealed with the temporary crown or healing abutments to contain the clot and/or bone graft and support the soft tissue. As previously mentioned, cement was extruded extraorally on an analog for cemented restorations to avoid the introduction of subgingival cement.
Postoperatively, patients were prescribed antibiotics and analgesics. Time was dedicated postsurgically for detailed verbal and written postoperative instructions specific to immediate implants and immediate provisional restorations with particular attention to eating instructions for the immediately provisionally restored implant sites to avoid premature loading. At 2 weeks, patients were seen for postoperative suture removal, review of home care, and reinforcement of instructions to avoid premature loading of the implants. Integration confirmation was scheduled between 3 to 4 months for mandibular implants and 5 to 6 months for maxillary implants.
Results
From February 1988 through December 2015, 13,630 implants were placed in 5,521 patients (3,159 women and 2,362 men).
• 7,340 of these implants were immediate implants in 4,270 patients (2,417 women and 1,853 men).
• 2,056 were IIIPR in 1,151 patients (902 women and 249 men).
• 5,284 were IINR in 3,119 patients (1,767 women and 1,352 men).
For the 2,056 IIIPR sites, regenerative protocols included:
• bone graft and membrane in two sites.
• bone graft alone in 91 sites.
• membrane alone in zero sites.
• no bone graft and no membrane in 1,963 sites.
Success was defined as successful osseointegration, successful bone regeneration, a steady state of bone and soft tissue under loading, and good esthetics. The success rate of immediate implants was 95.1%; the success rate of IIIPR was 95.0%; and the success rate of IINR was 94.9%. Average follow-up time to determine success was 5 years with a range up to 13 years for IIIPR and 26 years for IINR.
Case Example 1
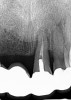
A 63-year-old woman presented with severe pain on biting of tooth No. 19 (Figure 1). Clinically there was pain on percussion and significant periodontal probing along the mesial root. The patient was anesthetized with infiltration anesthesia and the crown was horizontally sectioned from the lingual of the tooth. The remaining tooth was sectioned so the roots could be extracted individually. The socket was fully debrided and an implant was placed (Figure 2), which was prosthetically correct and stabilized in excess of 45 Ncm. The bone was milled to allow for unimpeded placement of a temporization abutment. The initial crown was revised to be the temporary crown in infraocclusion. Cement was extruded extraorally (Figure 3) prior to seating of the temporary restoration. The socket was sealed with the temporary crown and there were no sutures or bone graft (Figure 4 and Figure 5).
The patient was instructed in postoperative care specific to an immediately provisionally restored implant and an antibiotic and analgesic was prescribed. At 4 months, integration was confirmed. The patient was impressed for a final restoration that was cemented within 2 weeks. The final radiograph (Figure 6) and clinical photo (Figure 7) presents a 1-year postoperative demonstrating good esthetics, full bone regeneration, and a steady state of bone to the implant under loading.
Case Example 2
A 67-year-old woman presented on an emergency basis with a bad odor and taste from crown No. 12, which had been diagnosed that day at hygiene recall as decayed and no longer attached to the underlying root (Figure 8 and Figure 9). The patient was anesthetized and the existing bridge was sectioned (Figure 10), leaving crown No. 14 intact. The No. 12 root was extracted and the site was fully debrided of granuloma. A platform shift implant was stabilized in excess of 45 Ncm in position No. 12, which was prosthetically correct. The soft tissue of pontic site No. 13 was contoured to mimic soft tissue contours of a bicuspid and an implant was secured in excess of 45 Ncm. Implant No. 13 was milled to allow for unimpeded seating of the temporization abutment, whereas implant No. 12 did not need milling as it was a platform-shift implant. The existing crown No. 12 and cantilever No. 13 were revised to be a temporary bridge on Nos. 12 and 13 (Figure 11 and Figure 12). The revised temporary bridge was positioned in infraocclusion and cemented after the extrusion of excess cement extraorally (Figure 13). No bone graft or sutures were placed as the temporary crowns sealed the sockets.
The patient was prescribed antibiotics and analgesics and instructed in postoperative care particular to immediately provisionally restored implants. At 6 months, integration was confirmed (Figure 14) and the patient returned to her dentist for restoration. The implants were restored with individual cement-retained crowns with a platform shift for No. 12 restoration from the 6-mm diameter of the implant to a 5-mm diameter of the final restoration (Figure 15 and Figure 16).
Case Example 3
A 42-year-old man presented with a very loose bridge on Nos. 6 through 9 with periodontally compromised retainers on Nos. 6 and 9 (Figure 17 through Figure 19), and endodontically involved No. 10 with a calcified canal. Teeth Nos. 6, 9, and 10 were extracted, the sockets fully debrided, and pontic soft tissue on Nos. 7 and 8 sculpted to be symmetrical in soft tissue contour with the contralateral lateral incisor and central incisor locations. Implants were secured in position Nos. 6 through 10 (Figure 20) in excess of 45 Ncm, the bone was milled to provide unimpeded seating of temporary abutments, and temporary crowns were fabricated chairside and adjusted to be out of occlusion in centric relation and all excursions. The temporary crowns were cemented after extrusion of excess cement extraorally and the patient was prescribed antibiotics, analgesics, and instructed in postoperative care particular to immediately provisionally restored implants. At 6 months, integration was confirmed (Figure 20 through Figure 23) and after placement of scanning abutments, the implants and soft tissues were scanned. Final crowns were fabricated from the scanned images and were cemented after extrusion of excess cement extraorally (Figure 24 through Figure 26), and oral hygiene procedures were reviewed.
Discussion
Today it is possible to replace teeth with implants with one surgical procedure that is minimally invasive. The focus of this study was to evaluate the efficacy of IIIPR as a predictable protocol. In 2,056 implant sites, the treatment objective was accomplished as planned with the completion of an immediate implant with 99% flapless surgery and chairside fabrication of a temporary restoration. Very focused postoperative instructions were verbally reviewed so patients understood oral hygiene requirements and the need to avoid premature loading of the implant restorations. In two cases, the patients avulsed the implant and restoration with a daily very strong tongue manipulation and subsequently the need to avoid tongue pressure repeatedly on the restoration was included in postoperative instructions. Patients exhibited very little postoperative discomfort and were pleased to leave the office with an implant and restoration in place, and in most cases, there were no sutures. In those cases where the dimension of the restoration did not seal to the soft tissues, vicryl resorbable sutures were used to seal the soft tissue around the restoration and contain the clot. Patients were routinely seen at 2 weeks for reinforcement of home care and review of postoperative instructions when possible. In the presence of poor oral hygiene, patients were seen until home care was acceptable.
Across IIIPR cases, regenerative objectives were accomplished with good bone-to-implant volume and soft tissue maturation with two sites requiring a regenerative protocol of bone and membrane, 91 sites requiring bone graft alone, and the remaining protocols relying on normal socket regeneration. The two sites requiring membrane and bone were side-by-side implants in Nos. 8 and 9 where there was extensive infection, periapical granulomas, lack of labial plate, and required flap elevation with subsequent primary closure around the temporary restorations. The remaining 91 sites requiring bone grafts represented partial loss of labial or lingual plate, and fenestration defects were grafted from the osteotomy side of the defect with no flap reflection.
The variables in this study of external vs. internal abutment connection, screw vs. cement retention of provisional and/or final restorations, multiple adjacent vs. single implant sites, anterior vs. posterior implants, and maxillary vs. mandibular implants did not show statistically significant outcome differences. Flapless surgery did show heightened soft tissue and papillary retention, however, and was preferred by patients.
Outcome analytics provided data supporting the efficacy of IIIPR with a 95% success rate in 2,056 sites. IINR had comparable success rates. This data showed that the immediate restoration of an immediate implant does not contribute to a less favorable treatment outcome than immediate implant alone. In this population group, implant failure was primarily the consequence of compromised patient compliance where patients prematurely loaded the implant restoration.
We must be reminded that implant placement is a prosthetic event and that immediate implant surgery should only be employed if it satisfies the optimal prosthetic objectives of the case. In this implant population, the procedure was highly efficacious with less than 1% of sites found to be unfavorable for an immediate implant.
Final Thoughts
The outcome analytics from this study on IIIPR procedures suggests this protocol is highly successful and predictable. Immediate implant regenerative procedures are reproducible in diverse clinical situations. The time of extraction is the ideal time for implant placement and bone and gingival tissue regeneration and maturation because the implant surface is highly osteophilic. The immediate implant provides an ideal platform for esthetic tooth replacement. The temporary crown or healing abutment is a good scaffold for soft tissue development and maturation and for a socket seal to contain the bone graft or clot. The immediate implant accomplishes site retention and development in one procedure, minimizing the number of surgical procedures.
This protocol should be considered a patient-preferred approach in the transition from natural teeth to restored implants. Reducing multiple surgeries to one surgery, allowing patients to leave the dental office with an esthetically whole restoration in place, no displacement of soft tissue, and a normal sequence to prosthetic completion is a huge step forward in implant treatment.
Author Information
David A. Gelb, DDS, is a diplomate of the American Academy of Periodontology, a fellow of the Academy of Osseointegration, and a fellow of the American and International College of Dentists. Dr. Gelb has achieved global recognition as a leader in implant dentistry, and has pioneered surgical procedures for finite esthetics in implant dentistry, immediate implant placement, and bone regeneration. He lectures nationally and internationally and publishes extensively on implant dentistry. He is on staff at Hartford Hospital and has provided implant services in West Hartford for more than 25 years.
Acknowledgments
The author wishes to acknowledge the following colleagues for their prosthetic work: Drs. Susanne M. Gelb (case 1), Aaron Gross (case 2), and Abraham John (case 3).
Disclosures
David A. Gelb, DDS, is a co-developer of the Implant Tracker, which is sold by Implant Tracking Systems, LLC. He is also the developer of the Gelb Depth Gauge and has lectured on behalf of Nobel Biocare.
References
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
2. Laney WR, Tolman DE, Keller EE, et al. Dental implants: tissue-integrated prosthesis utilizing the osseointegration concept. Mayo Clin Proc. 1986;61(2):91-97.
3. Barzilay I, Graser GN, Caton J, Shenkle G. Immediate implantation of pure titanium threaded implants into extraction sockets [abstract 234]. J Dent Res. 1988;67:142.
4. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332-343.
5. Werbitt MJ, Goldberg PV. The immediate implant: bone preservation and bone regeneration. Int J Periodontics Restorative Dent. 1992;12(3):206-217.
6. Wohre PS, Schnitman PA, DaSilva JD, et al. Brånemark implants placed into immediate function: 5-year results. J Oral Implant. 1992;18:382.
7. Gelb DA. Immediate implant surgery: three-year retrospective evaluation of 50 consecutive cases. Int J Oral Maxillofac Implants. 1993;8(4):388-399.
8. Gelb DA, Lazzara RJ. Hierarchy of objectives in implant placement to maximize esthetics: use of pre-angulated abutments. Int J Periodontics Restorative Dent. 1993;13(3):277-287.
9. Rosenquist B, Grenthe B. Immediate placement of implants into extraction sockets: implant survival. Int J Oral Maxillofac Implants. 1996;11(2):205-209.
10. Schnitman PA, Wöhrle PS, Rubenstein JE, et al. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants.1997;12(4):495-503.
11. Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants. 1997;12(3):319-324.
12. Wöhrle PS. Single-tooth replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent. 1998;10(9):1107-1114.
13. Gelb DA. Immediate implant surgery: ten-year clinical overview. Compend Contin Educ Dent. 1999;20(12):1185-1192.
14. Misch CE, Wang HL, Misch CM, et al. Rationale for the application of immediate load in implant dentistry: part II. Implant Dent. 2004;13(4):310-321.
15. Wagenberg B, Froum SJ. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int J Oral Maxillofac Implants. 2006;21(1):71-80.
16. Jo DW, Yi YJ, Kwon MJ, Kim YK. Correlation between interimplant distance and crestal bone loss in internal connection implants with platform switching. Int J Oral Maxillofac Implants. 2014;29(2):296-302.
17. Chung SH, Park YS, Chung SH, Shon WJ. Determination of implant position for immediate implant placement in maxillary central incisors using palatal soft tissue landmarks. Int J Oral Maxillofac Implants. 2014;29(3):627-633.
18. Doan NV, Du Z, Reher P, Xiao Y. Flapless dental implant surgery: a retrospective study of 1,241 consecutive implants. Int J Oral Maxillofac Implants. 2014;29(3):650-658.
19. Peñarrocha-Oltra D, Peñarrocha-Diago M, Canullo L, et al. Patient-reported outcomes of immediate versus conventional loading with fixed full-arch prostheses in the maxilla: a nonrandomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(3):690-698.
20. Cooper LF, Reside GJ, Raes F, et al. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: a 5-year prospective evaluation. Int J Oral Maxillofac Implants. 2014;29(3):709-771.
About the Author
David A. Gelb, DDS
Diplomate, American Academy of Periodontology
Fellow, Academy of Osseointegration
Fellow, American and International College of Dentists
Private Practice
West Hartford, Connecticut