You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In the vast majority of initial dental appointments for a new patient, the first order of business is collecting proper intake forms, including the individual's personal information and medical and dental history. The next priority is diagnostics collection for the practitioner to properly assess the patient's condition and needs and to formulate an appropriate treatment plan. Soft tissues may be evaluated visually and palpated on examination. Hard tissues, however, such as the dentition and supporting bone anatomy, must be evaluated with the use of radiography. The level of penetration by x-ray transmission of the relative densities of hard tissues is measured when the effect of this radiation is "recorded" onto a surface that is sensitive to this radiation. An image is thereby obtained, by analog or digital means, and a determination is then made by the dental professional as to the condition of the tissue, healthy or pathologic, when the resulting image is viewed.1
Digital vs Analog Images
Radiographic images can be obtained on an analog x-ray film medium and properly processed for evaluation. Film radiography, however, is widely considered to be obsolete due to the need for chemical processing and storage issues, as well as time-sensitive decomposition of the small-size image.1,2
As is common in today's modern dental practice, a digital radiographic image can be exposed on the patient and visualized on a monitor viewscreen. The digital radiograph eliminates the need for those processes common to film, specifically: developing, fixing, drying and physical mounting. Bypassing these steps allows for a much faster image acquisition for the clinician's viewing, diagnosis, and treatment commencement. Digital radiography also improves safety by reducing radiation exposure to the patient by 25% to 50% in comparison to the fastest version of film.1,2
The traditional, outdated film radiographs always displayed a 2-dimensional view of the patient's anatomy. In contrast, digitally collected radiography provides either 2- or 3-dimensional imaging systems, the latter being an extraoral form of image collection as opposed to the intraoral radiography that is most widely used for initial patient evaluation.3
Anatomic, pathologic, and traumatic features can be initially identified in most cases by exposing and evaluating 2D intraoral radiographic images and subsequently ordering 3D studies when necessary. The 3D technological modality is known as cone beam computed tomography (CBCT).4-6The majority of developmental, restorative, surgical, prosthetic, and periodontal needs of patients on their initial evaluation, presumably by general dental practitioners, is accomplished with basic 2D digital intraoral dental radiography (DIDR).3
Digital Intraoral Dental Radiography
Two-dimensional DIDR is considered the diagnostic modality of choice for diagnosis and identification of dental caries, periapical (PA) pathology, natural dentition root morphology, periodontal condition, and endodontic canal anatomy.3Three-dimensional CBCT radiography is considered to be inappropriate as the initial imaging modality to address the preceding areas and should only be used in specific cases where symptoms or conditions warrant additional diagnostic information.5,6
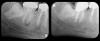
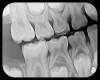
There are two specific types of DIDR sensor systems available to dentists in the marketplace: the hard-wired (HW) sensor and the photostimulable phosphor (PSP) sensor,1,2 also commonly known as phosphor "plates." A desirable feature common to both modalities is the ability to expose either bitewing (BW) or PA radiographic images. The BW radiograph (Figure 1) is usually considered more appropriate for caries detection, whereas the PA (Figure 2) is diagnostic for several different anatomic and pathologic issues.7
Hard-wired vs Photostimulable Phosphor Sensors
HW sensors present a "direct" image because they connect to a computer monitor with a wire and the image is available immediately after exposure. PSP sensors provide an "indirect" image because the sensor must be removed from the mouth after exposure and placed into a scanning unit for "reading" of the image stored on the sensor plate. This process is accomplished in seconds and is also considered to represent an expeditious workflow.1,2 The radiation necessary to create a diagnostic image is minimal in both systems; the difference between them is infinitesimal, and either technology represents a significant reduction in exposure to the patient compared with film radiographs.2,8
HW sensors have been observed to be used by the majority of dentists in North America,9presumably due to their immediate image acquisition. This modality has, however, demonstrated drawbacks and disadvantages in clinical practice, including much higher cost for HW sensors compared with PSP sensors; smaller surface area of HW sensors, requiring additional images and patient exposures compared with PSPs to capture an entire dentition; rigid, thick sensors that have been shown to cause patient discomfort and gag reflex, as well as inability for correct placement in posterior second and third molar areas; inability to capture apices of teeth and associated alveolar bone anatomy to monitor PA health; difficult use where palatal exostoses and mandibular tori are present; loss of cooperation when radiographs are needed on pediatric dental patients; and, finally, a very high need for retakes with the associated increase in radiation exposure, resulting in loss of time efficiency. In terms of thickness comparison, HW sensors range in thickness measurement from approximately 5.5 mm to as much as 8 mm or more, whereas PSP sensor thickness measures approximately 0.4 mm, allowing a better patient experience.9-13
PSP sensors are typically available in the three most common intraoral sizes: 0, 1, and 2, as well as the two less frequently used sizes available from some manufacturers, size 3 (for some BWs) and size 4 (for occlusal view images). The no. 0 size is considered most appropriate for PA imaging on pediatric dental patients, eventually advancing use to the no. 1 size as these patients grow and develop. The no. 2 size is most useful for all adult BW and PA radiographs and most pediatric BWs. When these no. 2 size BWs are properly placed and exposed, the developing succedaneous bicuspids and erupting second molars are usually visible to assure parents of the presence of these teeth in their children. Very few HW sensors, however, are sold in the no. 2 size. The most common size of HW sensor that is manufactured and sold is very similar in size to a no. 1 PSP. The cost of these reusable PSP sensors is minimal, and many individual PSP sensors can be stocked in the dental office for a tiny fraction of the cost of an HW sensor; therefore, it is economical for all the size choices to be made available for any patient needs. The replacement of a damaged PSP is also a tiny fraction of the cost for repair of a damaged HW sensor.2,9
PSP sensor technology offers many advantages to the clinician in patient retention and workflow. The most important consideration is patient comfort and cooperation. PSP sensors are wafer-thin and flexible to allow placement in positions to capture third molar images without gagging or pain. The larger surface area of the most popular no. 2 size PSP sensor allows images of more dental anatomy (Figure 3); therefore, fewer exposures are necessary to create a full-mouth radiographic series. Their flexibility allows placement around tori and exostoses.1,9-12 The bite blocks, stabilizers, BW tabs, and positioning rings that were used for film radiographs will easily accommodate PSP sensor placement.
The quality of the image obtained on the operatory monitor when comparing HW and PSP sensor results is similar.8,9 With retakes very rarely necessary, PSPs more closely conform to the radiographic rule of "As Low as Reasonably Achievable" (ALARA).1-3 Another very important concept for radiography best practices is the goal established by the organization known as the Alliance for Radiation Safety in Pediatric Imaging for clinicians to "Image Gently." This goal seeks to involve the dental professional to expose only diagnostically necessary radiographs on children to minimize the effects of ionizing radiation on especially susceptible developing tissues in their bodies.14,15 In this regard, PSP sensors allow greater patient cooperation, more comfort, better diagnostic imaging, fewer necessary exposures, and rare retakes.
Some representative radiographic PSP images are exhibited here for demonstration of the anatomy and pathology that can be visualized with this technology. Many of these images would not have been possible if HW technology were used (Figure 3 through Figure 8).
As displayed here, the 2D radiographic images in Figure 3 through Figure 8 can alert the clinician to the need for a further 3D CBCT analysis to properly ascertain the anatomy and extent of the pathology that is initially visible in the intraoral radiographs. Proper treatment or referral to the appropriate specialty practice can follow.5,6 No. 2 PSP radiographs, when used in a conventional full-mouth series of radiographs on a patient with a relatively complete dentition, will routinely allow visualization of the anatomy of third molars, mandibular canal, maxillary sinuses, full dental root morphology, and bone anatomy beyond the apices2,16,17 (Figure 9 and Figure 10).
Panoramic vs Periapical Radiography
Many clinicians have argued that the 2D diagnostic needs of dental professionals can be satisfied with panoramic rather than PA radiography. The drawbacks of panoramic radiography, when this extraoral modality is used in place of PA radiography, are evident in a number of clinical scenarios where visualization of subtle anatomic clues to pathologic conditions is not readily discernable, including diagnosis of caries and periodontal ligament width abnormalities. Endodontic cases are not easily treated with panoramic radiography because multiple views are necessary in the treatment phase, such as initial view, measurement image of root, master cone placement, and final image of the completed obturation. If a fistula is noted on examination, a gutta-percha point may be inserted into the fistula in order to determine which root or which tooth is infected when a PA pathosis is not easily located.17 Standing the patient upright and directing them away from the treatment operatory to a radiography room where a panoramic unit is located is highly disruptive to workflow, especially if a rubber dam and its associated clamp is in place for treatment.
Legal Ramifications of Insufficient Radiography
Incomplete and inadequate radiographic imaging can lead to errors and omissions in diagnosis and subsequent incorrect or substandard treatment, introducing iatrogenic results for patients and professional liability or licensure violation concerns for clinicians.18,19 State licensing boards commonly obligate the health professionals within their jurisdictions to maintain complete and accurate records. Deficient radiographic records can violate this requirement. In New York State, for example, the Rules of the Board of Regents specifies "failing to maintain a record for each patient which accurately reflects the evaluation and treatment of the patient" as one example of conduct that violates rules of licensure.19,20
In a case where a patient is unable to tolerate the correct placement of an HW sensor, either due to anatomic or behavioral reasons, in a location that will allow viewing the apex of a tooth to receive endodontic treatment, and subsequent post-obturation visits are periodically scheduled to follow the long-term outcome of the procedure, the inability to visualize an advancing PA lesion may constitute a charge of supervised neglect (Figure 11). The definition of supervised neglect is "a situation where a patient's oral health has been allowed to deteriorate over a period of time, despite regular attendances to the dentist who is responsible for the patient's care and treatment."21 Use of easily tolerated PSP radiographs in this instance would likely eliminate the potential legal difficulty by allowing the clinician to properly make the patient aware of any observed pathosis (Figure 12).
Pediatric patients and their parents also involve practical legal considerations associated with radiographic imaging. Here, the principles of ALARA and Image Gently are especially important because diagnostic clarity and complete disclosure of the dental condition of children to their parents must be achieved while care is taken to avoid unnecessary radiation exposure.14,15 The availability and low cost of PSP sensors in sizes 0, 1, and 2 imaging surfaces and ease of placement, to visualize the progress of the succedaneous dentition, makes a compelling case for pediatric use (Figure 13 and Figure 14) because full-mouth PA radiographic study is not always indicated in these young patients.
Conclusion
Two-dimensional DIDR imaging requirements in the majority of general and specialty dental practices concerned with the areas of diagnostic, restorative, periodontal, prosthetic, and surgical dentistry are best provided with PSP technology. In some cases, more advanced 3D CBCT radiographic imaging may be necessary, but initial needs are well served by PSPs because they can improve the quality of care, maximize patient cooperation, fulfill patient expectation, and help satisfy legal regulatory obligations.
About the Author
James G. Kouzoukian, DDS
Private Practice
Forest Hills, New York
References
1. Glazer HS. An update on digital radiography. Dental Learning. 2017;2-10.
2. Kouzoukian JG. Digital imaging: beyond radiography [lecture]. CDEWorld Updates in Clinical Dentistry Speaker Series; 2014-2015.
3. Bilski TM. CBCT for implant dentistry treatment planning [eBook]. CDEWorld. 2018;5(120):1-11. https://cdeworld.com/ebooks/cbct-for-dentistry-treatment-planning. Published October 15, 2018. Accessed September 10, 2020.
4. Baumgarten HS. Today's dental imaging: providing clinicians improved control over treatment. Compend Contin Educ Dent. 2015;36(10):776-777.
5. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics-2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508-512.
6. Kouzoukian JG. CBCT: standard of care in 3D imaging [lecture]. CDEWorld Updates in Clinical Dentistry Speaker Series; 2018.
7. Mark AM. Dental x-rays. J Am Dent Assoc. 2019;
150(7):636.
8. Farrier SL, Drage NA, Newcombe RG, et al. A comparative study of image quality and radiation exposure for dental radiographs produced using a charge-coupled device and a phosphor plate system. Int Endod J. 2009;42(10):900-907.
9. Christensen GJ. The clinical advantages of phosphor plate digital radiography. Clinicians Report. 2015;8(11):1,3.
10. Kaminer R. How to swiftly optimize your practice. Inside Dent. 2013;9(10):100.
11. Kouzoukian JG. You can't treat what you can't see: indispensable technology in digital intraoral radiography [webinar]. CDEWorld. https://cdeworld.com/webinars/21759-you-can-t-treat-what-you-can-t-see-a-preferential-technology-in-intraoral-radiography. Publish- ed June 2020. Accessed September 10, 2020.
12. Kouzoukian JG. Elevating diagnostics with PSP technology. Dent Prod Shop. 2020;14(4):34-35.
13. Kouzoukian JG. Peer to peer: indispensable for intraoral radiography. Inside Dent. 2020;16(7):40.
14. Farman AG. Taking the pledge to Image Gently. Inside Dent. 2014;10(9):17.
15. Alliance for Radiation Safety in Pediatric Imaging. Take the Image Gently pledge. www.imagegently.org. Accessed July 30, 2020.
16. Pryles RL. CBCT in endodontics: 3D diagnosis and treatment. Inside Dent. 2015;11(10):46.
17. Bahcall JK. Update on endodontic diagnosis. Inside Dent. 2015;11(10):52-55.
18. Christensen GJ. Ask Dr. Christensen. Dent Econ. 2009; 99(8):54-57.
19. Taxin C, Shub JL. Is SOAP your bread and butter? NYS Dent J. 2019;85(5):19-23.
20. New York State Rules of the Board of Regents. Section 29.2 General provisions for health professions. http://www.op.nysed.gov/title8/part29.htm. Accessed August 19, 2020.
21. Dental Protection. Undertreatment and supervised neglect. https://www.dentalprotection.org/uk/articles/undertreatment-and-supervised-neglect. Published August 31, 2014. Accessed August 19, 2020.