You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Restoring teeth with deep subgingival margins presents one of the greatest challenges in modern restorative dentistry.1,2These cases are complicated by limited access, the difficulty of achieving effective isolation, and the risk of violating the biologic width. Traditional approaches to addressing deep subgingival margins, such as crown lengthening or orthodontic extrusion, often require invasive procedures that come with significant anatomical and functional compromises, including attachment loss, exposure of root concavities, unfavorable crown-to-root ratios, and inferior esthetics, as well as increased treatment time and patient discomfort.3
As an alternative, the deep margin elevation technique was introduced in 1998 by Dietschi and Spreafico.4 Deep margin elevation, which is also known as coronal margin relocation or cervical margin relocation, is a minimally invasive method that involves repositioning deep subgingival margins coronally using composite resin.5 By transforming previously inaccessible margins into supragingival ones, deep margin elevation simplifies rubber dam isolation, facilitates impression making, and creates favorable conditions for bonding. This approach provides a conservative alternative to surgical interventions that aligns with the principles of minimally invasive dentistry.6,7
Despite its advantages, the application of deep margin elevation in clinical practice has been met with hesitancy. Limited long-term clinical studies and concerns about isolation, marginal adaptation, and microleakage contribute to its underutilization. Furthermore, properly adapting a matrix band to deep margins, especially in difficult cases, remains a persistent challenge. Improper adaptation of a matrix band can compromise the quality of the margin elevation and the final restoration, potentially leading to marginal leakage, secondary caries, and failure.8
To overcome these challenges in difficult cases of deep margin elevation, the use of a copper band in a so-called "matrix-in-matrix" technique offers a potential solution. Copper bands, which have been traditionally used in prosthodontics, are highly adaptable and can be molded to precisely fit the contours of the tooth, even in cases where the subgingival margin is irregular or deep. Their malleability allows for an exact fit, providing superior isolation and ensuring that composite resin can be applied without contamination. The tight seal created by the copper band prevents the ingress of fluids, such as saliva, crevicular fluid, or blood, which are major obstacles during deep margin elevation procedures.
In addition to aiding in isolation, copper bands help to better stabilize the restorative material during placement. Copper bands provide a rigid yet flexible matrix that supports the composite resin, ensuring proper adaptation to the tooth surface and reducing the risk of overhangs or voids. This is particularly advantageous in cases with irregular or compromised tooth structures where traditional matrix systems may fail to provide adequate support.
Combining deep margin elevation with copper bands offers a powerful approach for managing complex restorative cases involving deep margins. This technique not only preserves tooth structure and avoids the complications associated with surgical crown lengthening but also ensures that the restoration achieves optimal marginal integrity and longevity. Exploring the integration of copper bands into deep margin elevation procedures provides an opportunity to address the limitations of traditional approaches, improving both clinical outcomes and patient satisfaction.
Deep Margin Elevation
Deep margin elevation addresses the clinical challenge of managing subgingival margins, which are common in extensive Class II restorations or other scenarios involving deep proximal defects. These cases often complicate tooth preparation, isolation, impression making, and restoration placement. Traditionally, surgical approaches, such as crown lengthening or apical displacement of the soft tissues, were employed to make subgingival margins accessible. However, these procedures carry significant risks, including periodontal complications, sensitivity, and esthetic concerns, particularly in anatomically complex cases involving short root trunks, root concavities, or furcations.
Deep margin elevation offers a minimally invasive alternative that can eliminate the need for surgical intervention in many cases. In this technique, subgingival margins are relocated occlusally by placing a composite resin base, allowing for better isolation and access. This procedure has been refined over the years, and innovations such as immediate dentin sealing and advanced matrix systems have enhanced its efficacy. A critical component of deep margin elevation is achieving proper isolation and contouring, which is largely dependent on the choice of matrix.
Traditional curved or "banana-shaped" Tofflemire matrices are commonly used in deep margin elevation procedures due to their ability to provide an optimal gingival emergence profile and ensure proper adaptation; however, for margins at or near the cementoenamel junction, these matrices may fall short, particularly when managing very deep or irregular margins. In such cases, advanced matrix systems featuring a narrow design and lightweight structure can offer improvements in stability and adaptability. Nonetheless, certain cases remain problematic, and isolation and precise margin elevation are difficult to achieve with either traditional or modern matrix systems. For these challenging scenarios, the use of copper bands has shown potential as a superior approach for achieving reliable isolation and adaptation.
The Copper Band Technique
The use of copper bands in dentistry has a long-standing history that is rooted in their versatility and adaptability for managing challenging restorative cases. Historically, copper bands played a pivotal role in the creation of precise impressions, especially for teeth with extensive damage or irregular contours.9 By ensuring effective isolation and providing a stable working environment, they facilitated the production of high-quality impressions. Their effectiveness in gingival retraction further enhanced their utility, particularly in crown and bridge work, where achieving void-free impressions of subgingival areas was essential for successful restorations.10
Another significant historical application of copper bands was in placing large Class V amalgam restorations. In these cases, the copper band served as a "false wall," confining the amalgam material and enabling it to be compacted under pressure.11 This approach ensured a better seal and improved the durability of such restorations, which made it a valuable technique in restorative dentistry. Copper bands also proved indispensable for isolating severely broken or structurally compromised teeth during endodontic procedures.12 By creating a controlled and clean operative field, they reduced contamination and enhanced access, improving treatment predictability and success. For endodontically treated teeth that lacked coronal structure, copper bands were utilized in the fabrication of resin cores. Here, they served two purposes: providing isolation and acting as a matrix to shape the restoration. Available in various diameters and hardness levels, copper bands could be tailored to individual case requirements to accommodate complex anatomical challenges with ease.
The copper band's ability to minimize contamination from saliva and gingival fluids creates a controlled environment that is crucial for successful bonding and reducing the risk of restoration failure. The ability to mold the band to the cavity geometry helps in achieving a snug fit and minimizing gaps that could otherwise compromise the restoration. Unlike steel matrices, copper bands do not bond or stick to adhesive systems, which makes removal effortless, and their adaptability to various cavity shapes and sizes further enhances their versatility as an essential tool in restorative procedures. Copper bands are available in different thicknesses, and choosing the appropriate thickness for a given application is critical to its effectiveness. Commonly used thicknesses in dentistry are 5 mil (ie, 0.127 mm or 0.005 in), 3 mil (ie, 0.076 mm or 0.003 in), and 2 mil (ie, 0.051 mm or 0.002 in). Copper bands that are 5-mil thick provide greater rigidity and are suitable for larger cavities or when additional support is needed for material placement. Conversely, copper bands that are 3-mil or 2-mil thick offer greater flexibility, making them ideal for smaller cavities or complex anatomical shapes where precision is paramount. This range of options ensures that clinicians can select the right band thickness to meet the specific demands of each case. Copper bands are also often supplied as sheets that can be cut and shaped to fit individual cavities.
Copper Bands in Complex Cases
The following case examples demonstrate restorative scenarios in which copper bands can be incorporated to improve outcomes.
Canine Fossa: Effective Use of a Single Copper Band
The canine fossa, a distinct anatomical feature, is the concavity on the mesial crown and root surface of the maxillary first premolar (Figure 1). This concavity extends from the crown into the root trunk, distinguishing it from the convex mesial crown surface of the second premolar. Larger and deeper than the incisive fossa, the canine fossa is separated by the vertical ridge of the canine eminence, which corresponds to the canine tooth socket.
When cavity margins are located in the canine fossa due to caries, fractures, or cracks, the unique anatomy of this concavity poses a significant challenge (Figure 2 and Figure 3). Conventional matrix systems often fail to conform to its complex form and angles. This requires practitioners to possess expertise in adapting a customized matrix to suit the intricate contours of the fossa.
With its malleability and adaptability, a copper band offers an unparalleled solution for this purpose. It allows the practitioner to cut and shape the band to precisely match the unique structure of the canine fossa, accommodating variations in form and angles (Figure 4). Using a thicker copper band (ie, approximately 5 mil), provides the necessary strength to maintain stability during treatment. In addition, it effectively retracts the gingival tissue, which facilitates the placement and contouring of restorative materials, such as composite (Figure 5 and Figure 6).
Root Concavities: Sealing Defects With a Matrix-in-Matrix Approach
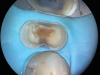
The root surfaces of maxillary molars present unique challenges due to their distinct anatomical concavities. On the mesial surface of the maxillary first molar, a pronounced concavity extends toward the furcation (Figure 7), whereas the distal surface features a broad and shallow depression that extends coronally to the cementoenamel junction. These concavities can pose significant difficulty in restorative procedures, particularly for deep Class II cavities, where their complex morphology complicates the adaptation of a single matrix (Figure 8).
To overcome these challenges, a matrix-in-matrix approach provides a reliable solution (Figure 9). The technique involves placing a circumferential matrix as a base, followed by a precision-shaped copper band with a thickness of 2 to 3 mil. The copper band conforms to the intricate contours of the concavities and serves as an auxiliary support. A liquid dam material is placed between the two matrices for added stability.
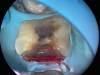
Extremely Deep Defects: Assisting Absolute Seal
In cases involving extremely deep defects that extend to the bone level, achieving an adequate seal and proper isolation for adhesive procedures can be particularly challenging (Figure 10 and Figure 11). Oftentimes, a single matrix proves insufficient to reach the depth of such defects and effectively shield the cavity from contamination by saliva or blood (Figure 12).
The matrix-in-matrix technique provides a practical and effective solution for these cases (Figure 13). By introducing a second matrix within the first, more specifically, a copper band that has been carefully cut and positioned inside a conventional matrix, the seal is significantly enhanced. This dual-layered approach not only extends the matrix coverage to the full depth of the defect for isolation but also ensures stability in the critical treatment area.
Conclusion
Having copper bands in the restorative armamentarium is invaluable for managing difficult and challenging cases, especially those involving deep subgingival margins and areas with complex morphology. Copper in sheet form enables customization into precise shapes for optimal adaptation, enhancing isolation, gingival retraction, and the stability of restorative materials during placement. Easily sourced from metal or hobby shops or online retailers, it can be sterilized and safely used in a variety of dental procedures to improve outcomes.
Queries regarding this course may be submitted to authorqueries@conexiant.com
About the Author
Masoud Hassan Zadeh, DDS
Private Practice
Drachten, Friesland,
Netherlands
Kiarash Karimi, DMD, DDS
Lecturer
UCLA
School of Dentistry
Los Angeles, California
Private Practice
Woodland Hills, California
References
1. Magne P, Harrington S, Spreafico, R. Deep margin elevation: a paradigm shift. Am J Esthet Dent.2012;2:86-96.
2. Kielbassa AM, Philipp F. Restoring proximal cavities of molars using the proximal box elevation technique: systematic review and report of a case. Quintessence Int.2015;46(9):751-64.
3. Magne P. M-i-M for DME: matrix-in-a-matrix technique for deep margin elevation. J Prosthet Dent.2023;130(4):434-438.
4. Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent.1998;10(1):47-54.
5. Hassanzadeh M. DME: deep margin elevation. In: Glossary of Biomimetic Restorative Dentistry. Kindle Direct Publishing; 2023:42-43.
6. Neymark A. An alternative to surgical crown lengthening margin elevation using a two-matrix system. Perio-Implant Advisory website. https://www.perioimplantadvisory.com/restorative-dentistry/article/16412250/an-alternative-to-surgical-crown-lengthening-margin-elevation-using-a-two-matrix-system. Published August 1, 2018. Accessed April 1, 2025.
7. Taylor A, Burns L. Deep margin elevation in restorative dentistry: a scoping review. J Dent. 2024;146:105066.
8. Scotti N, Baldi A, Vergano EA, et al. Tridimensional evaluation of the interfacial gap in deep cervical margin restorations: a micro-CT study. Oper Dent. 2020;45(5):E227-E236.
9. Small BW. Impression making with gingival hyperplasia using the copper band technique. Gen Dent. 2011;59(5):334-337.
10. Darby H, Darby LH 3rd. Copper-band gingival retraction to produce void-free crown and bridge impressions. J Prosthet Dent. 1973;29(5):513-516.
11. Alperstein KS. Copper band matrix for large Class V amalgam restorations. J Prosthet Dent.1995:74(3):305-308.
12. de la Peña VA, Darriba IL, Valea MC, Santana-Mora U. Use of a copper band to make resin cores in endodontically treated teeth lacking coronal structure. Oper Dent. 2015;40(5):458-461.