You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In modern dentistry, there has been a noticeable shift toward treatments that aim to preserve the natural structure of the tooth, especially when dealing with conditions such as caries or fractures. This approach contrasts with the more traditional methods, which often involved the removal of healthy tissue under the belief that doing so would help prevent future issues.1,2 These older methods, while once standard, are now being reconsidered in favor of more minimally invasive options. Air abrasion is one of the techniques that fits into this newer mindset of conservative treatment.
Historical Background
Air abrasion’s roots in dentistry began in the 1940s, when Robert B. Black, DDS, introduced the idea as a potential alternative to traditional rotary instruments for cavity preparation. His original concept involved using compressed air to propel aluminum oxide particles to effectively remove decayed tissue without generating heat or causing the vibrations typically associated with dental drills.2 At the time, however, the broader dental community was not yet prepared to adopt the method. There was a lack of adhesive restorative materials, and the principles of minimally invasive dentistry were neither well understood nor widely practiced.3 Nevertheless, Black’s pioneering set the stage for subsequent developments in conservative dental treatment.
By 1951, Black’s concept made it to the commercial market in the form of the Airdent system. It offered something different—a drill-free approach to cavity preparation—but it faced several limitations. One of the major drawbacks of the first air abrasion system was poor visibility: the spray of particles obstructed the clinician’s view of the working area. In addition, the device lacked precision in defining the internal shape of cavities. And because modern adhesive techniques were not available yet, dentists were still dependent on mechanical undercuts for retention. As a result of these early limitations, interest in air abrasion faded for a while. But in the 1990s, a turning point emerged. Advances in adhesive technologies and composite resins opened the door for a revival. Once bonding directly to enamel and dentin became more predictable, dentists could finally take full advantage of air abrasion’s conservative potential in restorative care.4
Aluminum Oxide: The Preferred Abrasive Medium
The material used in air abrasion plays a crucial role in its effectiveness.5 Out of the various material options that have been tested over the years, aluminum oxide (Al2O3), which is also known as alumina, has become the preferred choice for air abrasion. The preference for using alumina is largely due to its favorable balance of properties, which include that it is hard enough to cut effectively, that it is chemically inert, and that it is considered biologically safe.6 These qualities make it useful for removing decayed tooth material while helping to avoid harming the surrounding healthy tooth structure—an essential consideration in modern conservative treatments.
From what studies have shown, using alumina in this way doesn’t seem to compromise the bond to enamel or dentin, which is a key concern in restorative work.7 Other materials, such as bioactive glass, have been considered for air abrasion, especially because of its potential to promote remineralization, but alumina is still preferred in most cases, primarily because of its consistency and the familiarity that clinicians have with its clinical use.8
Air Abrasion’s Mechanism of Action
Air abrasion removes tooth structure by directing a focused stream of high-velocity abrasive particles, usually aluminum oxide, through a handpiece with compressed air, which allows for fairly precise removal of decayed or unwanted material. Comparable to sandblasting, air abrasion is used for a variety of purposes in dentistry, including cavity preparation and surface conditioning.9 The effectiveness of air abrasion can depend on a number of factors, including the particle size, the pressure used, and the exposure time.
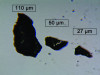
A study by Horiguchi and colleagues conducted in 1998 compared the cutting efficiency of various powders on enamel and dentin. They evaluated materials such as aluminum oxide, glass beads, crushed glass, and crushed polycarbonate resin.10 Interestingly, Horiguchi and colleagues found that angular crushed glass particles cut about three times more efficiently than round glass beads. This result showed how much of a difference that the shape and composition of the particles could make—not just in theory, but in real clinical application (Figure 1). It was one of several findings that helped to refine the technique moving forward.
The particle sizes used in air abrasion typically range from 27 to 110 µm, depending on the application (Figure 2 and Figure 3). This range has proven effective in creating the surface roughness necessary for restorative dentistry.5 When performing air abrasion, smaller particles are typically used for cleaning or polishing, whereas larger particles are more effective for cutting or removing tooth structure.11
Regarding the pressure used in air abrasion, higher pressure increases the speed and energy of the particles, increasing their cutting efficiency. However, the use of too much pressure can result in the removal of more healthy tooth structure than necessary as well as increase patient discomfort. Prolonged exposure carries the risk of deeper-than-intended abrasion. Therefore, it is critical to control both the pressure and the exposure time of the abrasive stream. By adjusting these factors, clinicians can fine-tune the procedure to ensure that only decayed tissue is removed and healthy tissue is left intact.
Clarifying the Terminology
The term air particle abrasion, which places more emphasis on the role that the abrasive particles play in the process, is often used interchangeably with air abrasion.4 Air abrasion is not limited to caries removal; it is also frequently used for surface treatments. For instance, it can be used to increase the surface area and energy of dentin and resin, thereby improving their bond strength.11 Relatedly, another widely used term is micro-etching, which refers to the microscopic roughness that air abrasion produces on tooth surfaces. Although the use of these terms may vary slightly in the literature, they generally refer to the same clinical technique.
Clinical Benefits
Air abrasion has become a well-established tool in dentistry, especially because it is more conservative than rotary instrumentation. It is mostly used for cavity preparation and removing early-stage decay, particularly when the damage is still minor. The key advantage of air abrasion is that it removes the decayed tissue while preserving the sound tooth structure, which helps to maintain as much of the natural tooth as possible.6,12 In addition, air abrasion produces less noise, vibration, and heat than traditional rotary instruments, and it can often be used without anesthesia, which is something that patients deeply appreciate.
Aside from preparing cavities, air abrasion has some other applications. For one, it is commonly used for surface treatments. It roughens tooth surfaces microscopically, which helps with bonding materials such as adhesives or sealants. Studies have shown that when air abrasion is combined with phosphoric acid etching, the bond strength of sealants is stronger than when acid etching is used on its own.13 It’s also good for removing superficial stains or old restorations. The precision of air abrasion allows dentists to target just the material that they want to remove without damaging the underlying tooth structure. This makes it an excellent option for cosmetic work, where preserving the natural tooth structure is key.14
When it comes to dentin, air abrasion can help create a rougher surface, which helps adhesives bond better.15-18 However, it is not without its drawbacks. Some research has shown that the process can leave behind a smear layer that clogs up the dentinal tubules with debris, and that may affect how the adhesive system interacts with the dentin.14 However, other research suggests that air abrasion can help reduce the smear layer while simultaneously roughening the surface of the tooth. This results in deeper resin tags, which has been shown to improve bond strength.19-22
Lastly, air abrasion has shown promise in treating cracks. One study that used optical coherence tomography to compare the effects of air abrasion and dental burs in treating deep cracks in dentin found that air abrasion results in fewer new cracks when compared to burs, which create vibrations that cause micro-cracking. This suggests that air abrasion might be a safer choice for managing cracks because it reduces the risk of further damage.23
Safety Considerations
Over the years, air abrasion has continued to evolve, but aluminum oxide remains one of the most reliable abrasives used in practice today. Although alternatives such as bioactive glass have been explored, aluminum oxide is still the preferred choice because of its hardness and consistent cutting ability, especially when working on enamel and dentin.11 Unfortunately, the fine particles released during air abrasion can become airborne, posing risks such as soft-tissue irritation or inhalation. To address concerns related to airborne particles, newer air abrasion devices have been developed with water spray functions. These improvements help reduce the amount of dust and debris floating around in the air. In addition, the water stream makes the abrasive jet more visible, which helps the operator accurately follow its direction and point of contact. Furthermore, the addition of water helps to prevent excessive heat buildup in the tooth. Despite these advancements, it is still crucial to use isolation techniques, such as rubber dams, and to rely on high-volume suction to keep the work area clean and safe (Figure 4 and Figure 5).
Conclusion
Aluminum oxide has remained a valuable material in restorative dentistry due to its efficacy in air abrasion techniques. Its ability to selectively remove decayed or damaged dental tissue while preserving healthy tissue aligns well with the principles of minimally invasive dentistry. Moreover, aluminum oxide effectively prepares enamel, dentin, and resin surfaces for adhesive procedures by creating a micro-roughened texture that enhances micromechanical retention. Therefore, air abrasion can play a critical role in a variety of treatments and should be considered a necessity for high-end restorative dentistry.
Queries regarding this course may be submitted to authorqueries@conexiant.com
About the Authors
Masoud Hassan Zadeh, DDS
Private Practice
Drachten, Friesland,
Netherlands
Scott Wolting, DDS
Private Practice
Heerlen, Limburg,
Netherlands
References
1. McComb D. Systematic review of conservative operative caries management strategies. J Dent Educ. 2001;65(10):1154-61.
2. Hegde VS, Khatavkar RA. A new dimension to conservative dentistry: Air abrasion. J Conserv Dent. 2010;13(1):4-8.
3. Berry EA 3rd, Eakle WS, Summitt JB. Air abrasion: an old technology reborn. Compend Contin Educ Dent. 1999;20(8):751-754, 756, 758-9 passim; quiz 764.
4. Banerjee A, Watson TF. Air abrasion: its uses and abuses. Dent Update. 2002;29(7):340-346.
5. Kim JE, Lim JH, Kang YJ, et al. Effect of pressure and particle size during aluminum oxide air abrasion on the flexural strength of disperse-filled composite and polymer-infiltrated ceramic network materials. Polymers (Basel). 2020;12(6):1396.
6. Eram A, Vinay Kr R, C KN, et al. Air-abrasion in dentistry: a short review of the materials and performance parameters. J Biomed Phys Eng. 2024;14(1):99-110.
7. Huang CT, Kim J, Arce C, Lawson NC. Intraoral air abrasion: a review of devices, materials, evidence, and clinical applications in restorative dentistry. Compend Contin Educ Dent. 2019;40(8):508-513; quiz 514.
8. Tan MH, Hill RG, Anderson P. Comparing the air abrasion cutting efficacy of dentine using a fluoride-containing bioactive glass versus an alumina abrasive: an in vitro study. Int J Dent. 2015;2015:521901.
9. Hassanzadeh, M. Glossary of Biomimetic Restorative Dentistry. Kindle Direct Publishing; 2023:2-3.
10. Horiguchi S, Yamada T, Inokoshi S, Tagmi J. Selective caries removal with air-abrasion. Oper Dent. 1998;23(5):236-243.
11. Kui A, Buduru S, Labune- A, et al. Air particle abrasion in dentistry: an overview of effects on dentin adhesion and bond strength. Dent J (Basel). 2024;13(1):16.
12. Laurell KA, Hess JA. Scanning electron micrographic effects of air-abrasion cavity preparation on human enamel and dentin. Quintessence Int. 1995;26(2):139-144.
13. Courson F, Renda AM, Attal J, et al. In vitro evaluation of different techniques of enamel preparation for pit and fissure sealing. J Adhes Dent. 2003;5(4):313-321.
14. Ferrazzano GF, Iodice G, Cantile T, Ingenito A. Scanning electron microscopic study of air abrasion effects on human dentine. Eur J Paediatr Dent. 2007;8(3):113-118.
15. Motisuki C, Monti Lima L, Emi Sanabe M, et al. Evaluation of the microtensile bond strength of composite resin restoration in dentin prepared with different sizes of aluminum oxide particles, using the air abrasion system. Minerva Stomatol. 2006;55(11-12):611-618.
16. França FM, dos Santos AJ, Lovadino JR. Influence of air abrasion and long-term storage on the bond strength of self-etching adhesives to dentin. Oper Dent. 2007;32(3):217-224.
17. Santos MJM, Costa MD, Rêgo HMC, et al. Effect of surface treatments on the bond strength of self-etching adhesive agents to dentin. Gen Dent. 2017;65(4):e1-e6.
18. Roque IA. Air abrasion effect on dentin bond strength: systematic review (master's thesis). Faculty of Medicine, University of Coimbra; 2020.
19. Los SA, Barkmeier WW. Effects of dentin air abrasion with aluminum oxide and hydroxyapatite on adhesive bond strength. Oper Dent. 1994;19(5):169-175.
20. Pilo R, Cardash HS, Oz-Ari B, Ben-Amar A. Effect of preliminary treatment of the dentin surface on the shear bond strength of resin composite to dentin. Oper Dent. 2001;26(6):569-575.
21. Chaves P, Giannini M, Ambrosano GMB. Influence of smear layer pretreatments on bond strength to dentin. J Adhes Dent. 2002;4(3):191-196.
22. Lankes V, Coldea A, Meinen J, et al. Airborne-particle abrasion vs. hydrofluoric acid etching of dental ceramics: impact on the tensile bond strength. Materials (Basel). 2024;17(23):5758.
23. Hovander D, Chyz G, Shimada Y, et al. Optical coherence tomography evaluation of deep dentin crack removal techniques. JADA FS. 2022;1:100012.