You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Disclosures: The authors had no disclosures to report.
Oral healthcare professionals are frequently required to select and prescribe analgesics to treat orofacial pain.1 Pain has both physiological and psychological elements. Poor pain management can result in patients who are difficult to manage, less likely to comply with prescribed treatments, and more likely to postpone or avoid dental visits. Appropriately selected medications that reduce orofacial pain improve clinical outcomes, making them an essential part of dental practice.2 Analgesic medications in dentistry are indicated for the relief of acute pain, postoperative pain, and chronic pain, and for controlling adjunctive intraoperative pain (ie, local anesthesia). In addition, when appropriately prescribed either preoperatively or intraoperatively, they not only mitigate pain but also reduce postoperative analgesic requirements.
Generally, two pathological processes are responsible for orofacial pain: 1.) tissue injury and inflammation (ie, nociceptive pain) or 2.) a primary lesion or dysfunction of the nervous system (ie, neuropathic pain).3 Accurately diagnosing the underlying pathophysiology, whether it is predominantly nociceptive, neuropathic, or a combination, is the first step in treating orofacial pain and selecting an appropriate medication with a mechanism of action that will target the root cause.4-6 Clearly defining the underlying pathophysiology of orofacial pain may be easy in cases of acute pain, such as a mucosal pain with proximate physical findings (eg, signs of tenderness, injury, inflammation) or a simple toothache; however, the diagnosis is more challenging if the pain is persistent and without a clear local cause (eg, myofascial pain or neuropathic pain).
Underlying Pathophysiology
Nociceptive orofacial pain is acute in nature and typically accompanies inflammation and tissue injury.1,6 Tissue damage stimulates the release of inflammatory mediators (ie, kinins, histamine, substance P, leukotrienes, prostaglandins), which initiate and magnify the pain impulses transmitted to the central nervous system, creating the perception of pain. Of these mediators, prostaglandins are most responsible for sensitizing neurons peripherally where the origin of the pain resides. They are also synthesized centrally in the higher brain centers where the pain is recognized. Finally, in response to pain impulses, prostaglandins recruit additional secondary neurons in the spinal cord and amplify pain sensitivity.
While nociceptive pain can spontaneously resolve if the underlying cause (eg, abscessed gingiva, inflamed pulp, carious lesion) is definitively treated, a pharmacological approach to pain management is the standard of care. Medications that target the synthesis of inflammatory mediators, such as prostaglandins, are some of the most effective analgesics in our armamentarium.
Medication Selection
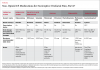
In medical practice, there is a commonly cited principle known as the “five rights” of medication administration (ie, right patient, right drug, right time, right dose, and the right route), which is verified to ensure medication safety.7,8 The drugs of choice for postoperative dental pain are presented in Table 1 through Table 3, including the nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen. The primary mechanism of action of these analgesics is to inhibit cyclooxygenase (COX) enzymes, which are responsible for the formation of prostaglandins from arachidonic acid.1,6 The other class of medications often employed in conjunction with these agents is glucocorticoids. Despite the fact that their biologic anti-inflammatory mechanism of action is still not completely understood, glucocorticoid medications such as dexamethasone have been utilized since the 1950s. In general, the glucocorticoids reduce blood levels of prostaglandins and leukotrienes, which are both involved in the pathogenesis of trismus, edema, and pain.9
Because opioid-based medications target the central mu opioid receptor and are not specifically anti-inflammatory agents, medications such as morphine, hydromorphone, and oxycodone should not be considered drugs of choice in treating dental pain secondary to inflammation. Instead, these analgesics should be reserved for a very small percentage of dental patients with severe, uncontrolled nociceptive orofacial pain, and even in such cases, they are best prescribed as combination products that contain an NSAID in addition to the narcotic moiety.2,10,11
Tramadol, a centrally acting analgesic thought to be a weak agonist of the mu opioid receptor and an inhibitor of serotonin and norepinephrine reuptake, was approved by the US Food and Drug Administration (FDA) in 1995 as an “atypical opioid” (Ultram®, Ortho-McNeil Pharmaceuticals Inc.). It was not originally classified as a controlled substance because it appeared to have a low risk for abuse or dependence. Although it offers less potential to cause respiratory depression at equianalgesic doses to opioids, unfortunately, tramadol still does not directly affect the primary mediator of acute dental pain: prostaglandins.12 Tramadol is also contraindicated in patients taking monoamine oxidase (MAO) inhibitors or patients with seizure disorders. For all of these reasons, tramadol should not be considered part of the standard armamentarium for the management of nociceptive orofacial pain.13,14
Aspirin and Related NSAIDs
Aspirin and the other NSAIDs specifically impede COX activity at the site of tissue damage, thus inhibiting prostaglandin formation peripherally, along the spinal cord, and in the higher brain centers. Although inhibiting this enzyme ameliorates the inflammatory triad of pain, inflammation, and fever, the conversion of arachidonic acid to cytoprotective prostaglandins is also impeded. For this reason, aspirin and other NSAIDs can cause adverse effects such as gastroduodenopathies, delayed wound healing, prolonged bleeding, and an increased risk of cardiovascular events.
In 2005, FDA began requiring manufacturers of prescription NSAIDs to include a black box warning and a medication guide with the package inserts for their products.15 The warning highlights the drugs’ potential to increase the risk of cardiovascular events and potentially life-threatening gastrointestinal bleeding. Designed to better inform patients about these risks, the medication guide accompanies every prescription NSAID at the time it is dispensed. The FDA also asked manufacturers of non-prescription, over-the-counter (OTC) NSAIDs to amend their labeling to include specific information about the potential gastrointestinal and cardiovascular risks and add information to assist consumers in the safe use of these drugs. In 2016, a meta-analysis concluded that patients taking routine NSAIDs to alleviate pain for ten days or less were not at an increased risk for adverse cardiovascular side effects.16
Concerns regarding the adverse effects of NSAIDs were also the impetus for the development of COX-2 selective NSAIDs such as celecoxib (Celebrex®, Pfizer Inc.). There are two well-described subtypes of COX enzymes: COX-1 and COX-2. COX-1 is a constitutive form that promotes hemostasis (ie, the synthesis of the prostaglandin analogue thromboxane A2, which increases platelet degranulation and adhesion), stomach mucosal integrity (ie, the synthesis of prostaglandins to protect against acid damage), and kidney function (ie, the synthesis of prostaglandins to help regulate normal renal blood flow). COX-2 is an inducible form that promotes the synthesis of proinflammatory prostaglandins and plays a significant role in mediating pain, inflammation, and fever. Selectively inhibiting COX-2 mitigates the inflammatory response, while neglecting COX-1 inhibition reduces the occurrence of adverse effects seen with traditional nonselective NSAIDS.
Acetaminophen
Acetaminophen is found as a single agent and in combination with other ingredients in OTC products and is commonly combined with narcotic agents in prescription products. In 2005, the most recent year for which figures are publicly available, US consumers purchased more than 28 billion doses of products containing acetaminophen.17 In general, acetaminophen is considered to be a safe medication, especially because it is associated with less cardiovascular, gastrointestinal, renal, and bleeding events when compared with the NSAIDs. However, hepatic injury resulting from acetaminophen use remains a serious health concern.18 As a result, in June 2009, an FDA advisory committee suggested new labeling and dosing guidelines for this ubiquitous analgesic.19 This language was updated in November 2015, requiring labels to state, “Liver warning: This product contains acetaminophen. Severe liver damage may occur if you take • more than 4,000 mg of acetaminophen in 24 hours • with other drugs containing acetaminophen • 3 or more alcoholic drinks every day while using this product.”20 In addition, FDA mandated that combination drug products not contain more than 325 mg of acetaminophen per tablet, capsule, or other dosage unit.21
While the dual COX model explains the differences between nonselective NSAIDs and COX-2 selective inhibitors, it does not explain the mechanism of action of acetaminophen. Acetaminophen’s efficacy profile resembles COX-2 selective inhibitors in that both display analgesic effects, antipyretic effects, and a relative lack of gastrointestinal toxicity; however, acetaminophen has a very weak anti-inflammatory action—an important characteristic of both nonselective NSAIDs and the COX-2 selective drugs.
There is a growing body of evidence in support of the existence of one or more additional subtypes of COX enzymes. A new COX-3 enzyme, which is produced by the same gene that encodes COX-1, was first described in the literature over 10 years ago.22-25 COX-3 is found in the brain and is inhibited by clinically attainable concentrations of acetaminophen. Although researchers are closer to understanding acetaminophen’s mechanism of action, debate continues regarding its primary site of action. While acetaminophen may alleviate pain by inhibiting prostaglandin synthesis via the COX-3 pathway, it may also work through the reversal of N-methyl-D-aspartate (NMDA), through an active metabolite that influences cannabinoid receptors, through substance P-induced hyperalgesia, or through the inhibition of nitric oxide pathways.26-28
Glucocorticoids
Produced by the adrenal glands and controlled by the hypothalamus, glucocorticoids are primarily involved with carbohydrate metabolism. Although the principal endogenous glucocorticoid is cortisol, others such as hydrocortisone, dexamethasone, methylprednisolone, and prednisone are more commonly used in dentistry as immunosuppressive agents (eg, for the treatment of erosive lichen planus and pemphigus vulgaris), anti-inflammatory agents (eg, for the treatment of mucositis and oral ulcerations), and analgesic agents (Table 3).29,30
In dentistry, the duration of glucocorticoid use is typically short. Although glucocorticoids act similarly to NSAIDs in that they inhibit the synthesis and release of inflammatory mediators, they differ in that they affect leukocyte function and become immunosuppressive with prolonged use. Short-term use lasting less than 7 days should not affect adrenal function or result in adverse effects or events.30 Patients who suffer from acute psychoses or exhibit a psychotic tendency should not receive a glucocorticoid. Additionally, these medications should be used with caution in patients with diabetes or peptic ulcerations and in pregnant or lactating females.31 Although glucocorticoids are known to have an effect on healing and bone remodeling, short courses of glucocorticoid therapy are not associated with wound disturbances or effects on the osseointegration of dental implants.32-36
The Perfect Prescription: 1 – 2 – 4 – 24
Ideally, selecting analgesics for the management of nociceptive orofacial pain is based on the patient’s medical history, the drug’s pharmacologic profile, the pain’s actual or expected intensity, the medication’s cost, the ease with which the medication can be obtained, and the anticipated patient compliance. It can be said that, “the medication that works is the one the patient takes.”
Ibuprofen was the first NSAID to demonstrate analgesic superiority over aspirin.37 A 400 mg dose has a greater peak analgesic effect and a longer duration of action than 600 mg to 1,000 mg of aspirin or acetaminophen or 60 mg of codeine and demonstrates comparable efficacy with traditional opioid analgesic combinations.38,39 Maximum anti-inflammatory action with ibuprofen may require higher doses (eg, 2,400 mg/day to 3,200 mg/day) than those indicated for effective analgesic action (eg, 200 mg to 600 mg 4 times per day; 1,200 mg/day to 2,400 mg/day).40,41 With a half-life of approximately 3 hours, ibuprofen should be administered every 6 hours to achieve steady-state blood levels.
In the average adult, analgesia from acetaminophen is readily measurable at a dose of 300 mg and plateaus at 1,000 mg.42 Acetaminophen follows first-order pharmacokinetics in the body (ie, metabolism and elimination are constant regardless of dose size), and similar to ibuprofen, it has a half-life of approximately 3 hours, so it should also be administered every 6 hours to achieve steady-state blood levels.43 The maximum effective dose of acetaminophen is two 500 mg tablets administered every six hours for a total of 4,000 mg per day.
The combination of acetaminophen and ibuprofen has previously been described by researchers in several studies and touted as an effective analgesic recipe.42,44,45 Because no marketed drug combination in the United States contains both an NSAID and acetaminophen, Dionne proposed taking the usual analgesic dose of ibuprofen (400 mg to 600 mg) every 4 to 6 hours, without exceeding 2,400 mg during a 24-hour period, as well as taking acetaminophen (650 mg to 1,000 mg) every 6 hours, without exceeding 4,000 mg in 24 hours.45 This combination of two medications (ie, ibuprofen 600 mg plus acetaminophen 1,000 mg) could be administered 4 times daily (every 6 hours) for 24 hours without exceeding the maximum daily dose of either drug (2 – 4 – 24).
If patients are compliant with these four doses of ibuprofen and acetaminophen, additional analgesics will likely not be required for oral pain management. The medications can be administered together every six hours or in a staggered fashion based on physician and patient preference. Following dental surgery, for patients in whom more frequent medication administration may be psychologically beneficial, the staggered approach may be desired despite the lack of pharmacological indication or benefit. Patient compliance and adherence with the prescribed regimen is vital to success. During the initial 24-hour postoperative period, patients should set alarms to fulfill their nighttime doses. After the initial 24-hour time frame, patients may opt to take the medications, either alone or in combination, on an “as needed” basis. If, despite excellent compliance, a patient’s pain level necessitates continued routine pain medication administration after 2 days following surgery, follow-up and reexamination by the oral healthcare professional is encouraged.
Analgesics can also be given preoperatively to mitigate postoperative pain (preemptive analgesia).46 This strategy could employ acetaminophen and/or an NSAID or a glucocorticoid where pain, swelling, and trismus are expected.47 Celecoxib (400 mg administered orally 30 minutes prior to the procedure) may be the most attractive NSAID for preemptive analgesia because, unlike the nonselective NSAIDs, it can mitigate the inflammatory response without delaying wound healing or prolonging bleeding.48 For patients who take anticoagulants such as warfarin, dabigatran, rivaroxaban, apixaban, or edoxaban, Celecoxib 200 mg given every 12 hours for the initial 24-hour postoperative period could also safely replace the postoperative ibuprofen 600 mg prescription.
The final ingredient for the perfect prescription (ie, 1 – 2 – 4 – 24) to treat nociceptive orofacial pain is adding a pre- or perioperative dose of the glucocorticoid dexamethasone. Several studies have demonstrated that a single 4 mg dose of dexamethasone can significantly reduce pain, swelling, and trismus following third molar surgery, implant surgery, and endodontic procedures.49-53 Dexamethasone is supplied as tablets, as an injectable, and as an elixir. If the 4 mg dexamethasone tablet is used, it is recommended to administer it either a day before or at the time of surgery. Alternatively, clinicians can submucosally inject 4 mg of dexamethasone perioperatively. This should be done adjacent to the surgical site in a manner consistent with an infiltration injection because the patient will be anesthetized in this area already. Dexamethasone injectable formulations come in several concentrations, but either the 4 mg/mL or 10 mg/mL concentration is recommended, which for this purpose would require 1 mL or 0.4 mL to be injected, respectively. While the choice between oral administration and submucosal injection is up to the clinician, submucosal injection is advantageous for several reasons. First, it does not require patient compliance, and second, it will not add additional discomfort because the medication is injected directly into the anesthetized tissue near the site of injury and swelling. In addition, submucosal injection offers a superior duration of action—6 days versus approximately 2.5 days for oral administration.54
Oral healthcare professionals can use the “1 – 2 – 4 – 24” mnemonic to help them remember the “perfect” analgesic formula: a single 4 mg dose of dexamethasone, either pre- or perioperatively, followed by a combination of ibuprofen 600 mg plus acetaminophen 1000 mg administered every 6 hours for 24 hours (ie, 1 single dose of dexamethasone, then 2 drugs, in 4 doses, for 24 hours).2
Conclusion
Acetaminophen is an effective analgesic with virtually no adverse effects except for those related to overdosing. Mild to moderate pain often responds to 650 mg of acetaminophen; however, 1,000 mg doses may be more effective for treating postoperative dental pain. Recommended doses of acetaminophen are not likely to cause hepatotoxicity in people who drink moderate amounts of alcohol, but they can become dangerous when patients take both acetaminophen and one or more combination products that contain acetaminophen. The efficacy of acetaminophen can be optimized when taken in combination with an NSAID such as ibuprofen.
Postoperative dental pain is caused by tissue injury and inflammation and usually has a short duration. As a result, a glucocorticoid followed by acetaminophen in combination with an NSAID should be considered the first line analgesic regimen for most patients. However, prescribers should always recommend the most effective analgesic regimen balanced against potential adverse events for the anticipated length of drug therapy.
References
1. Donaldson M, Goodchild JH, Wrobel MJ. Pharmacotherapy. In: Greenberg M, Glick M, Ship JA eds. Burket’s Oral Medicine, 12th Ed. Shelton, CT: PMPH USA; 2015:60-98.
2. Donaldson M, Goodchild JH. Appropriate analgesic prescribing for the general dentist. Gen Dent. 2010;58(4):291-297.
3. Fleming PS, Strydom H, Katsaros C, et al. Non-pharmacological interventions for alleviating pain during orthodontic treatment. Cochrane Database Syst Rev. 2016;12:CD010263.
4. Hersh EV, Kane WT, O’Neil MG, et al. Prescribing recommendations for the treatment of acute pain in dentistry. Compend Contin Educ Dent. 2011;32(3):22, 24-30.
5. Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. J Am Dent Assoc. 2013;144(8):898-908.
6. Aminoshariae A, Kulild JC, Donaldson M, Hersch E. Evidence-based recommendations for analgesic efficacy to treat pain of endodontic origin: a systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147(10):826-839.
7. Grissinger M. The five rights: a destination without a map. P T. 2010;35(10):542.
8. Goodchild JH, Donaldson M. Appropriate antibiotic prescribing for the general dentist. Gen Dent. 2009;57(6):627-634.
9. Esen E, Tas¸ar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg. 1999;57(10):1201-1206.
10. Dionne RA, Gordon SM, Moore PA. Prescribing opioid analgesics for acute dental pain: time to change clinical practices in response to evidence and misperceptions. Compend Contin Educ Dent. 2016;37(6):372-378.
11. Dionne R, Moore PA. Opioid prescribing in dentistry: keys for safe and proper usage. Compend Contin Educ Dent. 2016;37(1):29-32.
12. Gutstein HB, Akil H. Opioid analgesics. In: Hardman JG, Limbird LE, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 10th Ed. New York, NY: McGraw-Hill; 2001:590.
13. Medve RA, Wang J, Karim R. Tramadol and acetaminophen tablets for dental pain. Anesth Prog. 2001;48(3):79-81.
14. Edwards JE, McQuay HJ, Moore RA. Combination analgesic efficacy: individual patient data meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manage. 2002;23(2):121-130.
15. FDA announces important changes and additional warnings for COX-2s and NSAIDs. Pharmacist’s Letter/Prescriber’s Letter 2005;21(5).
16. Aminoshariae A, Kulild JC, Donaldson M. Short-term use of non-steroidal anti-inflammatory drugs and adverse effects: an updated systematic review. J Am Dent Assoc. 2016;147(2):98-110.
17. Acetaminophen overdose and liver injury—Background and options for reducing injury Page. https://www.fda.gov/ohrms/dockets/ac/09/briefing/2009-4429b1-01-FDA.pdf. Updated May 22, 2009. Accessed February 15, 2017.
18. Yoon E, Babar A, Choudhary M, Kutner M, Pyrsopoulos N. Acetaminophen-induced hepatotoxicity: a comprehensive update. J Clin Transl Hepatol. 2016;28;4(2):131-142.
19. Acetaminophen overdose and liver injury—Background and options for reducing injury. Available at: http://www.fda.gov/ohrms/dockets/ac/09/briefing/2009-4429b1-01-FDA.pdf. Accessed February 15, 2017.
20. Notice to Industry: Final Guidance for Over-the-Counter Products that Contain Acetaminophen Page. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm310469.htm. Accessed February 15, 2017.
21. Acetaminophen Prescription Combination Drug Products with more than 325 mg: FDA Statement - Recommendation to Discontinue Prescribing and Dispensing. Available at: https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm381650.htm. Accessed February 15, 2017.
22. Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18(10):915-921.
23. Botting RM. Inhibitors of cyclooxygenases: mechanisms, selectivity and uses. J Physiol Pharmacol. 2006;57 Suppl 5:113-124.
24. Hersh EV, Lally ET, Moore PA. Update on cyclooxygenase inhibitors: has a third COX isoform entered the fray? Curr Med Res Opin. 2005;21(8):1217-1226.
25. Chandrasekharan NV, Dai H, Roos KL, et al. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci USA. 2002;99(21): 13926-13931.
26. Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18(10):915-921.
27. Kis B, Snipes JA, Busija DW. Acetaminophen and the cyclooxygenase-3 puzzle: sorting out facts, fictions and uncertainties. J Pharmacol Exp Ther. 2005;315(1):1-7.
28. Graham GG, Scott KF. Mechanism of action of paracetamol. Am J Ther. 2005;12(1):46-55.
29. Sanghavi J, Aditya A. Applications of Corticosteroids in Dentistry. J Dent Allied Sci. 2015;4(1):19-24.
30. Becker DE. Basic and clinical pharmacology of glucocorticosteroids. Anesth Prog. 2013;60(1):25-32.
31. Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(4):406-415.
32. Corcoran T, Kasza J, Short TG, et al. Intraoperative dexamethasone does not increase the risk of postoperative wound infection: a propensity score-matched post hoc analysis of the ENIGMA-II trial (EnDEX). Br J Anaesth. 2017;118(2):190-199.
33. Bahammam MA, Kayal RA, Alasmari DS, et al. Comparison between dexamethasone and ibuprofen for post-operative pain prevention and control after surgical implant placement: a double-masked, parallel group, placebo-controlled randomized clinical trial. J Periodontol. 2017;88(1):69-77.
34. Thorén H, Snäll J, Kormi E, et al. Does perioperative glucocorticosteroid treatment correlate with disturbance in surgical wound healing after treatment of facial fractures? A retrospective study. J Oral Maxillofac Surg. 2009;67(9):1884-1888.
35. Fujimoto T, Niimi A, Sawai T, Ueda M. Effects of steroid-induced osteoporosis on osseointegration of titanium implants. Int J Oral Maxillofac Implants. 1998;13(2):183-189.
36. Keller JC, Stewart M, Roehm M, Schneider GB. Osteoporosis-like bone conditions affect osseointegration of implants. Int J Oral Maxilofac Implants. 2004;19(5):687-694.
37. Jasani MK, Downie WW, Samuels BM, Buchanan WW. Ibuprofen in rheumatoid arthritis. Clinical study of analgesic and anti-inflammatory activity. Ann Rheum Dis. 1968;27(5):457-462.
38. Cooper SA, Engel J, Ladov M, Precheur H, Rosenheck A, Rauch D. Analgesic efficacy of an ibuprofen-codeine combination. Pharmacotherapy. 1982;2(3):162-167.
39. Hersh EV, Moore PA, Ross GL. Over-the-counter analgesics and antipyretics: a critical assessment. Clin Ther. 2000;22(5):500-548.
40. Mehlisch DR. The efficacy of combination analgesic therapy in relieving dental pain. J Am Dent Assoc. 2002;133(7):861-871.
41. Ganzberg S. Analgesics: Opioids and nonopioids. In: Ciancio S, ed. ADA/PDR Guide to Dental Therapeutics. Chicago, IL: Thompson PDR Publishing; 2006:53-111.
42. Desjardins PJ, Cooper SA, Peripherally acting analgesics and antipyretics. In: Yagiela JA, Neidle EA, Dowd FJ, eds. Pharmacology and Therapeutics for Dentistry, 4th ed. St. Louis, MO: Mosby;1998:281-296.
43. Albert KS, Sedman AJ, Wagner JG. Pharmacokinetics of orally administered acetaminophen in man. J Pharmacokinet Biopharm. 1974;2(5):381-393.
44. Breivik EK, Barkvoll P, Skovlund E. Combining diclofenac with acetaminophen or acetaminophen-codeine after oral surgery: a randomized, double-blind, single-dose study. Clin Pharmacol Ther. 1999;66(6):625-635.
45. Dionne R. Additive analgesia without opioid side effects. Compend Contin Educ Dent. 2000;21(7):572-577.
46. Fletcher MC, Spera JF. Management of acute postoperative pain after oral surgery. Dent Clin North Am. 2012;56(1):95-111.
47. Pochapski MT, Santos FA, de Andrade ED, Sydney GB. Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):790-795.
48. Boonriong T, Tangtrakulwanich B, Glabglay P, Nimmaanrat S. Comparing etoricoxib and celecoxib for preemptive analgesia for acute postoperative pain in patients undergoing arthroscopic anterior cruciate ligament reconstruction: a randomized controlled trial. BMC Musculoskelet Disord. 2010;11:246.
49. Bahammam MA, Kayal RA, Alasmari DS, et al. Comparison between dexamethasone and ibuprofen for post-operative pain prevention and control after surgical implant placement: a double-masked, parallel group, placebo-controlled randomized clinical trial. J Periodontol. 2017;88(1):69-77.
50. Chen Q, Chen J, Hu B, Feng G, Song J. Submucosal injection of dexamethasone reduces post-operative discomfort after third molar extraction. J Am Dent Assoc. 2017;148(2):81-91.
51. Dan AE, Thygesen TH, Pinholt EM. Corticosteroid administration in oral and orthognathic surgery: a systematic review of the literature and meta-analysis. J Oral Maxillofac Surg. 2010;68(9):2207-2220.
52. Mehrvarzfar P, Shababi B, Sayyad R, Fallahdoost A, Kheradpir K. Effect of supraperiosteal injection of dexamethasone on postoperative pain. Aust Endod J. 2008;34(1):25-29.
53. Majid OW. Submucosal dexamethasone injection improves quality of life measures after third molar surgery: a comparative study. J Oral Maxillofac Surg. 2011;69(9):2289-2297.
54. Schull PD. Dexamethasone Sodium Phosphate. In: McGraw-Hill Nurse’s Drug Handbook. 2013. 7th Ed. McGraw-Hill Education; 2013:350-352.
About the Authors
Jason H. Goodchild, DMD
Associate Professor and Chairman
Department of Diagnostic Sciences
Creighton University
School of Dentistry
Omaha, Nebraska
Clinical Education Manager
Dentsply Sirona Restorative
Mark Donaldson, ACPR, PHARMD, FASHP, FACHE
Senior Executive Director
Vizient Pharmacy Advisory Solutions
Clinical Professor
School of Pharmacy
University of Montana
Missoula, Montana
Clinical Assistant Professor
School of Dentistry
Oregon Health & Sciences University
Portland, Oregon