You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The association between waterborne microorganisms and human disease caused by the contamination of water sources has been documented since the mid-1850s.1 Since then, a wide variety of both microscopic and macroscopic organisms have been shown to survive and proliferate in both natural water and manmade environmental systems (Table 1).2 Although established public health water treatment regulations (ie, filtration and chlorination) have been in effect for many years, waterborne infections and disease outbreaks continue to be reported from drinking water, recreational water, hospital water, and water used in healthcare-related devices. Extensive documentation of these types of infections can be found in the medical literature.3-8 Until recently, outbreaks and severe infections from contaminated water in healthcare settings were primarily reported in hospitals.
To put this public health issue into perspective for dentistry, it was not until 1963 that Blake first reported high concentrations of bacterial accumulation in coolant water for high-speed dental handpieces.9 Later investigations established that microorganisms in dental water delivery systems could form biofilms, leading to the proliferation of very high concentrations of bacteria. Subsequent studies have reported on the variety and nature of detectable microbial forms; mechanisms of microbial colonization in dental unit water lines (DUWLs) that form biofilms; potential infection problems that heavily colonized water can present for patients and dental healthcare providers; possible approaches for reducing microbial burden and maintaining safe, potable water for patient care; and the development of test systems to monitor the effectiveness of water treatment procedures.10-15
Most microorganisms detected in dental water systems originate from the public water supply and do not usually present a high risk of infection for healthy dental patients. However, several types of bacteria that are normally isolated from colonized dental unit water have the potential to cause infection and illness among immunocompromised patients. In recent years, the infection control challenge posed by contaminated DUWLs has shifted from "potential" to "documented" infection. Since 2011, one death of an elderly patient due to Legionella pneumophila16 and two outbreaks of Mycobacterium abscessus infections among pediatric dental patients have been reported after treatment with dental water that was heavily colonized with bacteria.16-18 Fortunately, continued progress to address this emerging problem has led to the development of multiple approaches aimed at reducing dental water colonization from environmental and human sources.
As more dental professionals adopt and routinely use available water treatment technologies, many are looking for assurance that they are using the products and performing the procedures correctly and asking questions concerning testing, including the following:
• What water monitoring systems are available to test microbial loads in dental unit water?
• Do these monitoring systems provide accurate and useful information concerning the effectiveness of a facility's treatment procedures?
• What are appropriate aseptic procedures when collecting water samples for testing?
The US Centers for Disease Control and Prevention, the American Dental Association, and other public health agencies recommend that any water used for routine dental procedures (ie, nonsurgical) should meet the US Environmental Protection Agency's (EPA) drinking water standard of less than 500 colony-forming units per milliliter (CFU/mL) of non-coliform heterotrophic bacteria.19-21 To meet this microbial threshold, dental facilities have been employing a combination of procedures, including using antimicrobial chemicals and technologies to control microbial colonization of DUWLs, flushing lines in the beginning of the day and after each patient, emptying lines overnight, and periodically applying DUWL "shock" treatments to augment routine treatment protocols.
The Basics of Water Line Testing
To ensure the safety of patients and dental professionals, every dental facility is responsible for meeting the minimum DUWL standards. Testing water lines is the most reliable way to confirm and document that dental water quality is acceptable. Many variables affect dental water quality and test results, and all of the methods currently used for dental water testing are inherently limited. Heterotrophic plate count (HPC) methods reveal only a fraction of the microorganisms in any water sample, and no single method will recover all microorganisms.21 Dental water testing is expected to detect elevated numbers from a spectrum of representative heterotrophic species for the purposes of confirming the success or failure of water line treatment and management.
DUWL testing captures and assesses waterborne species of planktonic heterotrophic bacteria to estimate the amount of contamination within the lines. Biofilm communities can change rapidly, which necessitates repeated testing to reliably monitor water quality over time. Many factors can affect DUWL test results, including movement of the tubing, water usage and flow, cycles of bacterial growth, and water line antimicrobial treatment.
Although scientific researchers can identify and enumerate waterborne microorganisms with great accuracy in laboratories, such processes are costly, time-consuming, and less practical for general DUWL testing. There is a need for affordable, efficient alternatives that can provide a meaningful assessment of water safety. Commercially available methods are designed to reduce cost and simplify the process by limiting parameters. When selecting a commercial water testing method, one should consider the types of organisms included and omitted, general efficacy (ie, capacity to grow and identify organisms), ability to correct for the effects of residual antimicrobial agents, time requirements, temperature requirements, technique difficulty, equipment needed, ease of interpretation, and the cost and practicality.
Basic options for water line testing include both in-office methods and mail-in water testing services offered by commercial laboratories. In-office testing methods are designed to avoid the complexity, cost, and time required by laboratory testing methods, but they have been found to be less reliable than the standard laboratory methods used by validated laboratories.21-23 Whatever the approach used, it should be designed to detect stressed organisms that are typically found in water lines being treated with commercial antibiofilm products. Although these organisms are difficult to detect and grow in their starved, inactive state, they can proliferate in exposed, susceptible hosts. Most water line treatment products add a low-level antimicrobial chemical to the dental treatment water to reduce the number of CFUs. The presence of residual antimicrobial chemical in the lines can affect test results by inhibiting bacterial growth during testing. In-office tests use water samples taken directly from dental tubing without dilution or filtration, whereas recommended laboratory testing methods filter and serially dilute samples to reduce the effects of any remaining antimicrobial products, allowing detection of these organisms.23
In-Office Water Line Testing
Several in-office water line tests (eg, HPC Total Count Sampler, MilliporeSigma; Aquasafe™ Water Test Kit, Pall Medical; Petrifilm™ AC Plate, 3M; Bacteria in Water Test Kit, Pro-Lab®) are available from dental supply companies. The HPC Total Count Sampler is a dip paddle containing a 0.45-µm filter and an absorbent pad with dehydrated agar medium in a plastic case (Figure 1). Dental unit water is poured into the case, and then the paddle is dipped into the water. After the paddle absorbs 1 mL of the liquid sample, the remaining liquid is discarded. The paddle is then incubated at room temperature for 7 days. The manufacturer states that accurate readings are possible up to 300 CFU/mL. In excess of this amount, the colonies grow together (ie, confluent growth) and the results become too numerous to count.
There is some evidence that the in-office methods underestimate water contamination.21 Researchers identify two key reasons for poor growth of DUWL heterotrophic bacteria on HPC Total Count Samplers: variations in room temperature (ie, 22° to 28° C) and omission of neutralization of the test sample. Dental water samples that contain residual antimicrobial agents should be neutralized to provide more accurate results. Despite this, HPC Total Count Samplers may be considered a useful gross screening method in situations involving low levels of contamination, such as in well-maintained and treated dental units.21,23,24
In-office testing places the burden of accuracy on office personnel, which requires training and dedication of time, space, and effort. Performing the testing protocol using an aseptic technique and adhering to the optimal bacterial growth schedule can pose a realistic challenge to dental teams. In addition, water line testing records and results should be kept as part of the written safety program. With these considerations, regular in-office testing can provide a rough estimate of bacterial load and identify overgrowth events during ongoing water line management procedures.
Mail-in Water Line Testing Processes
Professional laboratories control many of the variables in the water testing process, which improves the reliability of their results. Laboratories employ trained technicians who work under controlled conditions with regulated equipment. Sample processing on R2A agar using standard plating method 9215C is considered the gold standard for enumerating common heterotrophic bacteria in potable water. Standard method 9215D adds filtration and dilution steps to neutralize water line antimicrobials. Mail-in laboratory testing services that use these serial plating processes with low nutrient R2A agar, low incubation temperatures, and 5 to 7 days of incubation time yield a more accurate (usually higher) plate count than in-office methods.21,24,25 Sterile vials, a cold pack, and a box are provided by the laboratory, and sample collection and shipping are managed by the customer. The samples must be shipped overnight, and results are ready after approximately one week of incubation (Figure 2).
Dental facilities should attempt to avoid the common errors that undermine water line management efforts by using commercially available water line antimicrobial products with recommended shocking procedures, carefully following the manufacturer's instructions, and regularly testing their water lines. Different lines in dental units have exhibited varied potential for biofilm accumulation and should be tested accordingly. Mail-in laboratories provide supplies and instructions along with guidance and consulting to assist offices in meeting recommended water line safety standards. Evidence shows that after a frequent (ie, quarterly) testing protocol is established, compliance improves to a more than a 90% pass rate (ProEdge, unpublished data).
Why and When Should DUWLs Be Tested?
The recommendation to test DUWLs is targeted towards verifying the effectiveness of existing water line management programs and confirming the continuous potability of water used in treatment. Unfortunately, errors may occur when there are undetected problems in efforts to control water line biofilms, which can lead to the failure of management procedures. Researchers have previously reported audits of DUWLs that revealed that up to 50% of treated lines failed to meet potablility standards. They suggested that implementation of a monthly testing protocol could improve compliance.23
To provide more information about dental offices that currently test their water lines, two dental water testing laboratories (ie, the Sterilization Assurance Service at Loma Linda University and ProEdge Dental Water Labs) were consulted. Both laboratories provided generalized assessments based on 10 years of water testing, and ProEdge Dental Water Labs provided anonymous data from 22,196 consecutive test results. These water line testing results were evaluated, and the pass and fail rates were compared based on the various types of devices or lines, the water line antimicrobial product used (or named by the dental office), and the number of tests performed (ProEdge, unpublished data).
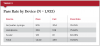
Pass Rate by Device
One analysis compared the test results from samples taken from different devices or types of lines. According to the results, 76.25% of air/water syringe hoses passed and 75.84% of handpiece hoses passed, but only 60.68% of scaler hoses passed. The average pass rate for all types of lines was 74.50% (Table 2).
Although every DUWL should be tested, testing every port may be overly costly and time intensive. As alternatives, strategies for selecting representative ports or determining sequences for rotational testing protocol have been suggested, especially after ongoing testing repeatedly indicates acceptable water quality (ProEdge, unpublished data; M. Rust, personal communication, January 2018). If a rotational testing protocol is considered, it may be advisable to test infrequently used lines as well as frequently used lines. In addition, samples from more than one DUWL from a single source (ie, reservoir) may be combined for testing. If contamination is detected, lines should be re-treated and individually retested to determine which are affected (S. Mills, personal communication, April 2018).
Pass Rate by Antimicrobial Product Type
In addition to the comparison of test results for different types of water lines, the test results of lines using various treatment protocols were compared. Table 3 presents field data accumulated from thousands of dental facilities. The data reflect potential misuse of the individual products. Failed water tests are typically corrected after identifying mistakes such as not following the manufacturer's instructions and not shocking on a regular basis.
The data reveal that periodic shocking combined with daily antimicrobial treatment using tablets yielded the highest pass rate (88%) and appears to be the most reliable, current long-term protocol. The average pass rate for all water that was treated with any commercially available DUWL treatment product was found to be 69%. Shock treatments alone, without continuous water line treatment, resulted in a 60% pass rate, and using a daily treatment product without shocking yielded a 58% pass rate.
Although there are numerous options for daily water line cleaners, there are only two main options for performing shock treatments: bleach (diluted to a concentration of 1:13 for a maximum 10-minute contact time) and commercially available shock treatment products designed specifically for shocking DUWL (left in lines overnight, according to the manufacturer's directions). Scientific literature supports the use of both options; however, bleach is more likely to damage dental unit components over time (M. Rust, personal communication, January 2018; S. Mills, personal communication, April 2018). Using bleach in DUWL is an off-label use of the product and is inconsistent with its EPA registration (S. Mills, personal communication, April 2018).
Pass Rate by Number of Tests
An important point noted by both laboratories was that water line samples from their customers often reveal high levels of contamination initially, but those levels improve after repeated testing. In one analysis of 3,742 samples (Table 4), only 67% of the water samples passed (< 500 CFU/mL) on the first test, but results improved after repeated testing. After five repeat tests, 92% of the samples met potable water standards.
Water line testing must be continued over time because resistant biofilm species may still rebound after several years of constantly using some DUWL antimicrobial products. Both of the laboratories interviewed offer consultation services, which they partially credit with improved water quality and test results. Improved water test results are considered confirmation that the antimicrobial product, equipment maintenance, protocol, technique, and overall compliance are successful. Keeping water line test results as a record of compliance with safety standards can provide a facility with ongoing documentation of their efforts in this area (W. Zhang, personal communication, April 2018; M. Rust, personal communication, January 2018).
Understanding the possible reasons for poor test results can aid in revising and improving a facility's DUWL treatment protocols. Before beginning water line testing, safety managers can assist in avoiding typical errors by addressing and correcting common problems. Management factors that are necessary for controlling water line contamination and ensuring good test results include the following:
Manufacturer's directions must be followed. This includes instructions for regular shock treatments, correct dilution of antimicrobial products, correct sequencing or frequency of water treatment, and emptying water bottles or drying lines, as recommended. All DUWLs should be shocked periodically with an appropriate chemical to remove biofilm. Water line products retard, but do not prevent, biofilm growth. Biofilm builds up slowly and must be removed. Weekly shock treatments are recommended if a continuous antimicrobial product is not used; however, less frequent shock procedures may still be necessary when continuous antimicrobials are in place. Water line testing can determine the need for and optimal time interval for shocking, even when the manufacturer's directions for a facility's antimicrobial product exclude shocking instructions (W. Zhang, personal communication, April 2018; M. Rust, personal communication, January 2018; S. Mills, personal communication, April 2018).
Source water should be clean. Distilled water, in-office distillers, and reverse-osmosis units may become contaminated over time. Filtered or processed water should be tested because filters can become contaminated as well. Municipal tap water may contain organisms that proliferate in DUWLs, and "hard" water with a high concentration of total dissolved solids (TDS) can interfere with the efficacy of water line treatment products. These contaminants in source water can potentially exhaust the active ingredients of antimicrobial products before water line microbes are neutralized. It should be noted that TDS filters do not filter out microorganisms.
DUWLs should be flushed at the beginning and end of the day and between patients. Flushing is recommended to remove contaminated fluids after periods of stagnation and after possible infiltration of patient-derived contaminants.
Shocking should not be confused with flushing. Shocking is the process of treating DUWLs with strong chemicals that detach biofilm from the internal surfaces. Flushing involves running treatment water through open ports of DUWLs, which removes fluids but will not reliably remove attached biofilms.
DUWLs should be tested consistently. The performance of consistent DUWL testing can be used to confirm the effectiveness of a facility's maintenance protocol and help determine the proper frequency of shock treatments.
Conclusion
To meet regulated water standards, dental facilities must treat and regularly test their DUWLs. Testing is the most reliable way to discover problems with dental water quality and provides documentation of compliance. Test kits for in-office use and mail-in testing services are available to provide a means for dental facilities to assess the effectiveness of their water treatment protocols. Although these products and services may become more user-friendly as new equipment management options and test methods emerge, to properly protect patients and dental professionals, dental facilities must understand how to properly treat water and correctly perform DUWL testing.
About the Authors
Nancy Dewhirst, RDH, BS
Adjunct Faculty Member
West Coast University
Anaheim, California
John Molinari, PhD
Professor Emeritus
University of Detroit Mercy
School of Dentistry
Detroit, Michigan
References
1. Snow J. On the mode of communication of cholera. In: Clendening L, ed. The Sourcebook of Medical History. New York, NY: Paul B. Hoeber, Inc.; 1942:468-472.
2. Molinari J. The ongoing challenge of waterborne infections. Inside Dent. 2017;13(8):52-58.
3. Craun GF, Brunkard JM, Yoder JS, et al. Causes of outbreaks associated with drinking water in the United States from 1971 to 2006. Clin Microbiol Rev. 2010;23(3):507-528.
4. Hlavsa MC, Roberts VA, Kahler AM, et al. Outbreaks of illness associated with recreational water-United States, 2011-2012. MMWR Morb Mortal Wkly Rep. 2015;64(24):668-672.
5. Rutala WA, Weber DJ. Water as a reservoir of nosocomial pathogens. Infect Control Hosp Epidemiol. 1997;
18(9):609-616.
6. Decker BK, Palmore TN. The role of water in healthcare-associated infections. Curr Opin Infect Dis. 2013;26(4):345-351.
7. Kanamori H, Weber DJ, Rutala WA. Healthcare outbreaks associated with a water reservoir and infection prevention strategies. Clin Infect Dis. 2016;62(11):1423-1435.
8. McClung RP, Roth DM, Vigar M, et al. Waterborne disease outbreaks associated with environmental and undetermined exposures to water-United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66
(44):1222-1225.
9. Blake GC. The incidence and control of bacterial infection of dental units and ultrasonic scalers. Brit Med J.1963;115:413-416.
10. Martin MV. The significance of the bacterial contamination of dental unit water systems. Brit Dent J. 1987;163(5):152-154.
11. Williams JF, Johnston AM, Johnson B, et al. Microbial contamination of dental unit water lines: prevalence, intensity, and microbial characteristics. J Am Dent Assoc. 1993;124(10):59-65.
12. Karpay RI, Plamondon TJ, Mills SE, et al. Comparison of methods to enumerate bacteria in dental unit water lines. Curr Microbiol. 1999;38(2):132-134.
13. Mills SE. The dental unit water line controversy: defusing the myths, defining the solutions. J Am Dent Assoc. 2000;131(10):1427-1441.
14. Mills SE. Dental unit water and air quality challenges. In: Molinari JA, Harte JA, eds. Cottone's Practical Infection Control in Dentistry. 3rd ed. Philadelphia, PA: Wolters Kluwer; 2010:63-75.
15. Gruninger SE. Disease transmission through dental unit water: an update. ADA Professional Product Rev. 2014;9(2):8.
16. Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit water line. Lancet.2012;379
(9816):684.
17. Peralta G, Tobin-D'Angelo M, Parham A, et al. Notes from the field: mycobacterium abscessus infections among patients of a pediatric dentistry practice - Georgia, 2015. MMWR Morb Mortal Wkly Rep. 2016;65
(13):355-356.
18. American Dental Association. Nontuberculous mycobacterial infection linked to pulpotomy procedures and possible dental water line contamination reported in California and Georgia. https://www.ada.org/en/science-research/science-in-the-news/nontuberculosis-mycobacterial-infection-linked-to-pulpotomy-procedures. Published September 21, 2016. Accessed May 15, 2018.
19. Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health care settings-2003. MMWR Recomm Rep.2003;52(RR-17):1-61.
20. Kohn WG, Harte JA, Malvitz DM, et al. Guidelines for infection control in dental health care settings-2003. J Am Dental Assoc. 2004;135(1):33-47.
21. Porteous N, Sun Y, Schoolfield J. Evaluation of 3 dental unit water line contamination testing methods. Gen Dent. 2015;63(1):41-47.
22. Cohen ME, Harte JA, Stone ME, et al. Statistical modeling of dental unit water bacterial test kit performance. J Clin Dent. 2007;18(2):39-44.
23. Lal S, Singhrao SK, Brickness M, et al. Monitoring dental-unit-water-line output water by current in-office test kits. Curr Microbiol. 2014;69(2):135-142.
24. Momeni SS, Tomline N, Ruby JD, Dasanayake AP. Evaluation of in-office dental unit water line testing. Gen Dent. 2012;60(3):e142-e147.
25. Reasoner DJ. Heterotrophic plate count methodology in the United States. Int J Food Microbiol. 2004;92
(3):307-315.