You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
A developmental anomaly or the presence of perio-dontal disease can cause the bone surrounding some teeth to undergo alterations that result in osseous defects.1 For example, a palatogingival groove is an anomaly of enamel formation that predisposes the teeth to severe bony defects.2 The palatogingival groove facilitates bacterial colonization of the gingival complex, leading to periodontal inflammation, epithelial attachment breakdown, and progression to a periodontal pocket with bone loss.3 The management of a palatogingival groove presents a challenge to most clinicians because it requires an interdisciplinary approach to diagnosis and treatment planning.4 If a palatogingival groove is not diagnosed in time, collaborative management may require an endodontist and a periodontist to resolve concerns in these areas prior to restoration by a restorative dentist.
The correct diagnosis of a palatogingival groove can only be made after a detailed clinical exam and proper documentation. Clinical exam for a suspected palatogingival groove should include photographs as well as 2- and/or 3-dimensional x-ray imaging to characterize defects in the skeletal morphology and any previous restorative work. Attam and colleagues reported that the prevalence of palatogingival groove was approximately 2.8% to 8.5%.5 The presence of a palatogingival groove predisposes a tooth to periodontal breakdown because it is plaque-retentive. Occasionally, palatogingival grooves are associated with pulp necrosis and an endodontic-periodontal lesion, which is a challenging condition to diagnose and treat.6
Esthetic restoration of the maxillary anterior dentition involves issues that often require a combined periodontal/restorative team therapy, including attention to treatment planning, treatment sequencing, diagnostic wax-ups, and effective interdisciplinary communication.7 Other considerations in maxillary anterior rehabilitative work include achieving the appropriate size, shape, and proportion of the teeth and periodontium.8
The following case provides evidence for the successful management of a palatogingival groove as it relates to localized, severe chronic periodontal disease.
Case Report
Diagnosis and Treatment Planning
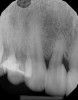
A 45-year-old female patient was referred to our office for the treatment of bleeding gums and sensitivity associated with tooth No. 7. Clinical and radiographic evaluations revealed highly inflamed tissues, easily provoked bleeding, and edematous palatal gingival tissue supporting tooth No. 7 (Figure 1 and Figure 2). Crowding, a widened periodontal ligament, dens in dente, deep probing depths, bleeding on probing, dilacerations, missing papilla, and angular bone loss were also observed, indicating that tooth No. 7 had a poor prognosis. The groove began at the cingulum and formed a deep fold of enamel that extended to the coronal third of the root. This radicular groove disrupted normal periodontal attachment and caused a self-sustaining, progressive localized periodontal pocket to form. The groove also presented a potential pathway for bacterial penetration into deeper parts of the root, which could lead to endodontic involvement if left untreated.6
Clinical Treatment
The patient was premedicated with an antibiotic (ie, clindamycin 150 mg; orally, three times daily) and an analgesic (ie, Motrin 800 mg; three times daily, as needed). To enable access to the root and bony defects, two vertical incisions were made on the midpalatal aspects of teeth Nos. 6 and 8 and horizontal incisions were made from tooth No. 6 to tooth No. 8 using a No. 12 scalpel blade (Carbon Steel, Benco Dental). This flap reflection enabled the visualization of significant bone loss and missing palatal plates on tooth No. 7. The magnitude of the gingival groove (ie, length and depth) was also evaluated prior to elimination. Using a fine diamond bur, the large fold of enamel extending to the coronal third of the root was reduced and the deep grooves were eliminated. After the bony defect on the midpalatal and mesial aspect of tooth No. 7 was grafted with particulate freeze-dried bone allograft (Cortical bone, Maxxeus Dental) and covered with a resorbable membrane (Bio-Gide®, Geistlich Pharma North America, Inc.), the flap was closed with PGA sutures (Figure 3 through Figure 5).
After 4 months, when the patient had no more bleeding or sensitivity, prosthodontic treatment was initiated to correct the crowding, facilitate normal hygiene, and enhance the patient's smile.
Discussion
The proposed treatment was tailored and coordinated based on the specifics of the patient's diagnosis. The importance of early diagnosis and management remained the focus, using odontoplasty to eliminate the palatogingival groove. The pulp was not involved. This was followed by periodontal regenerative therapy to reduce the size of the pocket and regenerate lost bone, thus creating a healthy environment for crown placement.After resolving the pain associated with tooth No. 7, the treatment also facilitated a broader approach to enhancing the patient's smile by correcting the crowding. This approach was desired by both the patient, who wanted to become disease free before addressing other issues, and the restorative dentist, who wanted the restoration placed in a healthy environment. A coordinated, interdisciplinary approach worked well and put smiles on the faces of everyone involved.
An alternative treatment option involved removing tooth No. 7 and replacing it with a dental implant. However, because implant complications are on the rise, maintaining the natural teeth by providing quality dental care has been recommended by Giannobile and Lang,9 who caution against extracting teeth with endodontic or restorative problems. Instead, they recommend preserving patients' natural dentition, emphasizing that this is a skill that our profession should not lose.
Conclusion
The combination of periodontal regenerative therapy for angular bone loss on the mesial aspect of tooth No. 7 and odontoplasty on the palatal aspect, provides a predictable method to manage palatogingival groove. This is especially true if the developmental anomaly is detected early enough to save the tooth (ie, prior to endodontic involvement). In this case, despite a poor prognosis due to long-standing periodontal inflammation, tooth No. 7 could be saved. In addition, endodontic treatment was avoided and the neighboring tooth (ie, No. 8) benefited from periodontal treatment. This approach is supported by the literature, which describes teeth with deep palatogingival grooves being treated collaboratively and saved successfully using a combination of endodontic therapy, surgical enucleation, odontoplasty, and periodontal regenerative treatment.1,10,11 The early diagnosis of disease is important in rectifying the periodontal condition and delivering quality dental care to avoid tooth loss and the need for implant placement. Even after being compromised, successfully treated natural teeth last longer than implants.12 Biologic and prosthetic complications are common with implants,13 and their treatment is not predictable.14,15 Most patients are emotionally attached to their front teeth and do not want to lose them. Psychological elements are the main predictors of a patient's decision to seek dental therapy.16 In this case, the patient wanted to improve her esthetics after saving tooth No. 7. To correct for crowding, improve her smile, and restore the teeth to proper form and function, the patient preferred prosthodontic treatment over orthodontic treatment.
Reevaluation of this case 3 years posttreatment (Figure 6) revealed normal probing depths, no bleeding on probing, a significant improvement in the angular bone loss on tooth No. 7 (Figure 7), and a stable periodontal condition. Prosthodontic treatment was delivered in a healthy environment and provided a stable occlusion and a satisfying overall appearance (Figure 8 through Figure 10). Preservation of this esthetic outcome was a motivating factor for the patient to maintain a high standard of oral care. For financial reasons and in consideration of her low smile line, the canines were not involved in the prosthodontic therapy.
The patient was happy about her decision to accept periodontal treatment and appreciated the teamwork between the surgeon and the general practitioner. Specialists and general dentists should explore their options for interdisciplinary treatment on a case-by-case basis and work together to achieve cost-effective outcomes that keep everyone smiling.
About the Author
Ahmad Soolari, DMD, MS
Private Practice
Silver Spring, Maryland
References
1. Sharma S, Srivastava D, Sood V, et al. Endodontic and periodontal management of a severely affected maxillary lateral incisor having combined mucosal fenestration and palatogingival groove. J Indian Soc Periodontol. 2015;19(3):348-351. doi: 10.4103/0972-124X.152413.
2. Garrido I, Abella F, Ordinola-Zapata R, et al. Combined Endodontic Therapy and Intentional Replantation for the Treatment of Palatogingival Groove. J Endod. 2016;42(2):324-328. doi: 10.1016/j.joen.2015.10.009.
3. Gupta KK, Srivastava A, Srivastava S, et al. Palatogingival groove - a silent killer: Treatment of an osseous defect due to it. J Indian Soc Periodontol. 2011;15(2):169-172. doi: 10.4103/0972-124X.84388.
4. Castelo-Baz P, Ramos-Barbosa I, Martín-Biedma B, et al. Combined Endodontic-Periodontal Treatment of a Palatogingival Groove. J Endod. 2015;41(11):1918-1922. doi: 10.1016/j.joen.2015.08.008.
5. Attam K, Tiwary R, Talwar S, et al. Palatogingival groove: endodontic-periodontal management--case report. J Endod. 2010;36(10):1717-1720. doi: 10.1016/j.joen.2010.06.025.
6. Sooratgar A, Tabrizizade M, Nourelahi M, et al. Management of an Endodontic-Periodontal Lesion in a Maxillary Lateral Incisor with Palatal Radicular Groove: A Case Report. Iran Endod J. 2016;11(2):142-145. doi: 10.7508/iej.2016.02.014.
7. Rada RE. Interdisciplinary management of a common esthetic complaint. Gen Dent. 2014;47(4):387-389.
8. Polack MA, Mahn DH. Biotype change for the esthetic rehabilitation of the smile. J Esthet Restor Dent. 2013;25(3):177-186. doi: 10.1111/jerd.12029.
9. Giannobile WV, Lang NP. Are dental implants a panacea or should we better strive to save teeth? J Dent Res. 2016;91:5-6.
10. Kishan KV, Hegde V, Ponnappa KC, et al. Management of palato radicular groove in a maxillary lateral incisor. J Nat Sci Biol Med. 2014;5(1):178-181. doi: 10.4103/0976-9668.127322.
11. Rajput A, Talwar S, Chaudhary S, et al. Successful management of pulpo-periodontal lesion in maxillary lateral incisor with palatogingival groove using CBCT scan. Indian J Dent Res. 2012;23(3):415-418. doi: 10.4103/0970-9290.102243.
12. Holm-Pedersen P, Lang NP, Müller F. What are the longevities of teeth and oral implants? Clin Oral Implants Res. 2007;18 Suppl 3:15-19.
13. Derks J, Schaller D, Håkansson J, et al. Effectiveness of Implant Therapy Analyzed in a Swedish Population: Prevalence of Peri-implantitis. J Dent Res. 2016;95(1):43-49. doi: 10.1177/0022034515608832.
14. Carcuac O, Derks J, Charalampakis G, et al. Adjunctive Systemic and Local Antimicrobial Therapy in the Surgical Treatment of Peri-implantitis: A Randomized Controlled Clinical Trial. J Dent Res. 2016;95(1):50-57. doi: 10.1177/0022034515601961.
15. Jepsen K, Schneider E, Dommisch H, et al. Management of a Central Incisor with Horizontal Root Fracture for Esthetic and Functional Rehabilitation. Int J Periodontics Restorative Dent. 2016;36(1):65-73. doi: 10.11607/prd.2338.
16. Grzić R, Spalj S, Lajnert V, et al. Factors influencing a patient's decision to choose the type of treatment to improve dental esthetics. Vojnosanit Pregl. 2012;69(11):978-985.