You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Silver is one of the "precious" metals. Designated by the symbol Ag on the periodic table of elements and known also as argentum, its atomic number is 47.1 It is malleable, ductile, resistant to oxidation from the atmosphere, and polishable to a high luster. When alloyed with other metals, such as copper and gold, the resultant materials are more fusible and exhibit increased toughness and hardness, making them ideal for coinage, ornaments, and jewelry.1 No metal has a higher thermal or electrical conductivity; therefore, silver is used in printed electrical circuits and as a coating in electronic conductors. Silver also forms compounds with other elements, such as silver chloride (AgCl), silver iodide (AgI), and silver bromide (AgBr)-all of which are used in photography and photographic paper.1
Silver and the compounds it forms have a toxic effect on algae, fungi, and bacteria in vitro, which usually carries over in vivo. This antimicrobial action is related to the ability "of the biologically active silver ion to irreversibly damage key enzyme systems in the cell membranes of pathogens, and this explains the metal's long history as an antimicrobial agent in healthcare."2 Silver has been used in water purification, wound care, bone prostheses, reconstructive orthopedic surgery, cardiac devices, catheters, and surgical suturing and appliances.2,3
Alexander extensively reviewed the history of silver in medicine.4 He noted that Cyrus the Great, the founder of the first Persian Empire, who ruled from 550 bc to 530 bc, and other Persian kings used silver vessels for their drinking water. They did not know about microbes, but they did recognize that the water stayed fresh in those containers.4 Alexander also noted that Hippocrates (460 bc to 377 bc) used silver preparations to treat ulcers and promote wound healing and that silver nitrate was mentioned as a medical preparation in a pharmacopeia published in Rome in 69 bc.4
Restoring Teeth With Silver
The history of silver as a dental filling material can be traced back to the Tang Dynasty, when it was mentioned in a medical text by Su Gong in 659.5 In addition, Czarnetzki and Ehrhardt wrote about silver fillings that were rendered in Germany in 1528.6 In 1830 or thereabouts, amalgam became the dental restorative material of choice due to its low cost, ease of application, strength, and durability. What followed was approximately 190 years of use that, although significantly diminished, continues to this day. Silver amalgam filling materials have undergone continuing alterations of the mercury, silver, tin, copper, and zinc content, and advancements in the manufacturing methods have continued to improve the physical characteristics of silver amalgam and maximize its longevity in the mouth.7,8 The use of silver amalgam has always been accompanied by controversy, some of which is based on science and some not.8,9
Early Uses of Silver Nitrate
Later in history, silver nitrate (AgNO3) became extensively used for bacteria control in both medicine and dentistry. The use of silver nitrate for oral conditions can be traced back to 1827. In 1847, D. Francis Condie reported that "nitrate of silver was the only local remedy employed in the cases of gangrene of the mouth that occurred in the Children's Asylum of Philadelphia from June 1st, 1827 to January 1st, 1830, the greater portion of which terminated favourably. As soon as the disease of the mouth was detected, the nitrate of silver, either in pencil or solution, was applied, freely, to the parts affected."10 In 1850, Chapin A. Harris recommended that "spongy gums that manifest no disposition to heal, their edges should be touched with a solution of the nitratum argentum (ie, silver nitrate), which will seldom fail to impart to them a healthy action."11 He also cautioned practitioners to keep the solution from "getting into the fauces, as in that case, it will cause a disagreeable nausea." In the 20th century, silver nitrate was perhaps most widely recognized for its use in treating newborns' eyes to prevent ophthalmia neonatorum; however, erythromycin ointment is now the antibiotic generally used for that purpose. Currently, silver nitrate sticks are used for the treatment of common warts, and the compound is also used for other antiseptic and antimicrobial purposes.
The use of silver nitrate to chemically alter the course of dental caries infections has a history dating back to the mid-19th century. In 1846, the German dentistry publication Zahnarzt presented a clinical tip, giving directions on how to use "hollenstein" (ie, hellstone, devil's stone, lunar caustic, argerol, silver nitrate) for the treatment of dental caries lesions.12 The article (translated into English) addresses the use of "hellstone in heavily eroded teeth. If the tooth, as is usually the case with damp tooth decay, is so heavily eroded that it can no longer be sealed, yet one still wishes to keep it, one may try the following method by which one at least stops the decay and preserves the tooth as long as possible. One is to carefully scrape out the decay and dampen the inside with a very concentrated silver nitrate solution or with moistened silver nitrate powder."12 The article also notes that "a tooth cared for in this manner will often be preserved for years without being sealed, without being damaged in any way by eating or drinking. However, if one still wishes to seal such a hollow tooth, then it is good to first apply the procedure just cited, namely to scrape out the decay and apply silver nitrate to the substance (ie, any remaining decayed tissue); the seal will then last much longer."12
Silver Nitrate Gains Momentum
Although some suspect that silver nitrate had been used for the treatment of tooth decay prior to 1846, strong evidence of such activity is not well documented in the literature. However, there have been many writings regarding silver nitrate since 1846. Prinz wrote that "Clark, Chupein, Shanasy, Tomes, Salter, Bauer, Black, Miller, Pierce, Conrad, and many others-have greatly lauded the value of silver nitrate as a means of abating the progress of dental caries, and especially Taft."13 Willoughby D. Miller, in his many writings and, especially, in his classic text, revolutionized scientific thought about the microbiological etiology of dental caries and had a major influence on the researchers of his day and beyond.14 He wrote about chemical methods of altering intraoral microflora to influence soft-tissue and osseous pathosis and the pathogenesis of dental caries. Pedley, in his 1895 book addressing the diseases of children's teeth, made six different references to the use of "lunar caustic" (ie, silver nitrate) for treating tooth sensitivity and caries lesions.15
According to Duffin, Percy Howe's article in Dental Cosmos about using silver nitrate for chemical treatment of dental caries16was "the most highly regarded dental scientific paper of his era." Duffin pointed out that the silver nitrate solution described by Howe was so popular for about 30 years after 1920 that it was referred to as "Howe's solution."17 Duffin also reported that Howe was the first research director of Boston's Forsyth Institute and noted that "thousands of children who were treated at the institute every year received the silver nitrate method and this was carefully documented in the Forsyth annual records. Additionally, Army soldiers leaving for WWI were also treated with Howe's solution."17
Greene Vardiman Black offered an erudite and detailed discussion of the use of silver nitrate for dental caries in primary teeth and for Class V cervical caries in permanent teeth, which also demonstrated the compound's black stain characteristic in the mouth.18 In a 1924 revision of Black's text, Arthur Black joined his father in documenting the use of silver nitrate as a chemical means to treat dental caries infections.19 Also in 1924, Hogeboom's text advocated for silver nitrate use,20 and in 1937, McBride's book pictured an example of a black stain resulting from silver nitrate treatment.21 Decades later, in their 1956 textbook, Muhler and Hine presented a 50- year history of the use of silver nitrate for the treatment of dental caries lesions.22
Silver Diammine Fluoride
The most common contemporary use of silver in dentistry involves the treatment of caries with silver diammine fluoride (SDF) (ie, AgFH6N2). Regarding its chemistry, SDF has been described as a metal ammine complex of silver fluoride. Its ligands are ammonia, thus "ammine" is the appropriate spelling; however, the term "amine" is very commonly used incorrectly in the nomenclature for this chemical.23
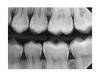
SDF was developed in Osaka, Japan, in 1969.24,25 During the next 5 decades, its use and related research spread around the world.26-32 Various formulations of SDF (Bioride®, Densply Industria e Comericio Ltda; e-SDF™, Kids-e-Dental Llp; Riva Star, SDI; Saforide®, Toyo Seiyaku Kasei Ltd) have been developed in different countries to attenuate dental caries infections. In 2014, an SDF solution made up of 62% water, 25% silver, 8% ammonia, and 5% fluoride (Advantage Arrest® Silver Diamine Fluoride 38%, Elevate Oral Care, LLC) was the first to gain approval by the US Food and Drug Administration to be used in the United States as a tooth desensitizing agent33; however, others have since been cleared as well. Its ability to affect dental caries pathodynamics has developed into an exceedingly popular off-label use by dentist clinicians. Figure 1 depicts an example of a malformed and carious permanent first molar that had been treated with SDF followed by 2.5% sodium fluoride varnish 6 months and 12 months prior when it was only partially erupted. This strategy attenuated the caries infection for over a year, until the patient, an extremely anxious 7-year-old boy, was able to tolerate routine restorative treatment.
Designating 38% SDF as a "caries arresting" agent is problematic. The term "arrest" suggests that the microbes within a treated caries lesion are stopped. The perception that caries lesion infections are arrested by application of SDF is based on "the surface hardness and visual characteristics of the caries lesion, the desensitizing ability of the SDF, and the erroneous belief that the low concentration of silver ions thoroughly kills high concentrations of microbes."34 However, that is not true. A team of research scientists at TRAC Research has shown that "recovery of a high number of viable microbes throughout SDF treated lesions indicates significant doubt that silver diamine fluoride arrests dental caries lesion progression."34 One month after three weekly, two-minute SDF treatments were performed on a caries lesion, the TRAC researchers were able to use anaerobic and aerobic incubation to grow and identify a variety of microorganisms, including Actinomyces sp, Actinomyces odontolyticus, Actinomyces oris, Atopobium sp, Eikenella corrodens, Gemella morbillorum, Gemella sanguinis, Lactobacillus fermentum, Micromonas micros, Rothia dentocariosa, Rothia mucilaginosa, Staphylococcus epidermidis, Streptococcus sp, Streptococcus gordonii, Streptococcus mitis/oralis, Streptococcus mutans, Streptococcus parasanguinis, Streptococcus salivarius, Streptococcus sanguinis, Streptococcus sobrinus, Streptococcus tigurinus, Veillonella sp, Veillonella parvula, and Veillonella rodentium.34
The TRAC researchers concluded that "currently, there is no dental product or treatment that arrests dental caries progression-the best outcome possible today is delay of progression."34 SDF intercepts and slows down the progress of a caries infection lesion, and its fluoride component, plus additional fluoride from a fluoride varnish cover, serve to remineralize the tooth structure. Relief from tooth sensitivity also is achieved. The TRAC researchers identified special indications for the use of SDF, including the following34:
•The presence of caries in very young and very old patients for whom the minimization of trauma and pain are important
•Cases involving difficult behavior or medical management
•Cases involving access to care problems, such as bedridden elderly
•Identification of caries in demineralized tooth structure
SDF in Practice
Although the TRAC research is most telling regarding the action of 38% SDF on the microflora of caries lesions, practical experience using multiple applications of SDF for carious primary teeth, which are repeated at varying intervals after initial placement (eg, 2, 3, or 6 months), demonstrates that it clearly augments attenuation of the infective process, oftentimes until primary tooth exfoliation.35,36 One wonders what would be revealed by microbiological studies of caries lesions that were treated more frequently or using a longer application time than 2 minutes. It is logical that different treatment protocols will result in different degrees of reduction of microbial numbers and virulence, but the ideal treatment regimen may vary for different patients as well as for different caries lesions in the same patient. The best SDF regimen for any one patient may also be influenced by a dental clinician's experience, purpose, and intuition. In an interview in 2017, Rella Christensen offered a remarkable summary of the clinical use of SDF.37
In the primary dentition, improving access to caries lesions by trimming the enamel and/or selectively debriding a certain amount of carious substance will improve the coverage and penetration of SDF solution.35,36 These procedures do not involve local anesthetic injections or discomfort to the patient. Such methods of SDF application could perhaps be applied to the treatment of incipient pit and fissure caries in permanent posterior teeth as an interim caries control measure. Certainly, 38% SDF solution is ideal for caries disclosure because the infected regions turn black and the healthy tooth structure does not.
There are other indications for SDF in pediatric dentistry, including intercepting early proximal caries lesions in primary and permanent teeth using soft dental pick delivery,35,38 controlling caries lesions in primary teeth that will exfoliate naturally within a year or two, and intercepting caries lesions at the margins of dental restorations rather than replacing those restorations.39 In patients for whom treatment is influenced by financial or management considerations, SDF can provide a useful delaying tactic to intercept caries progression until traditional restorative methods can be accomplished. Likewise, for geriatric patients, SDF caries attenuation can be a useful continuing option to rapidly and comfortably end a dental caries crisis. A search of the medical and dental literature and the internet identified many dozens of modern research and clinical reports, technique articles, review papers, and opinion pieces on SDF.40-52
With the introduction of SDF to the North American dentistry marketplace, the concept of chemical management of dental caries using silver materials in conjunction with the preventive abilities of systemic and topical fluorides has been vigorously rejuvenated, particularly in pediatric and geriatric dentistry. An excellent example of this was how the atraumatic restorative treatment (ART) concept was evolved into the silver-modified atraumatic restorative technique (SMART). The ART procedure involves the use of hand instrumentation to achieve partial debridement of a caries lesion after cleaning the treated tooth. Next, polyacrylic acid is scrubbed into the lesion, after which it is rinsed with water and the moisture is blotted. A glass polyalkenoate (ionomer) restorative cement (not resin-modifed, so as to maximize the fluoride dynamics) is then placed and isolated while hardening.53,54No local anesthetic or powered instrumentation is used. The SMART procedure also involves the use of hand instrumentation to partially debride a caries lesion, but prior to restoration, the lesion is soaked in SDF for 2 minutes.53 Although this method does not replace traditional restorative dentistry protocols, in certain cases, it can offer a practical treatment alternative for dentists, to the benefit of patients, especially in parts of the world where electricity and modern dentistry equipment are not available.
Silver Nanoparticles
A contemporary overview of the uses of silver in dentistry would be incomplete without mention of silver nanoparticles, which range in size from 1 nm to 100 nm. Callister and colleagues recently provided an excellent outline of the nature of silver nanoparticles, how they are synthesized, and their mechanisms of action.55 The article describes the antimicrobial action of silver nanoparticles, how they disrupt biofilms and act in caries control, and their anti-inflammatory effects. In addition, Callister and colleagues review how remineralization and demineralization are influenced by silver nanoparticles and emphasize that rewetting agents, sealants, cements, resin-based composites, and gutta percha can be improved because silver nanoparticles "have the ability to deter bacterial microleakage and adherence and reduce matrix metalloproteinase interactions in bonded restorations."55
Conclusion
When one considers that the concept of using common silver nitrate to alleviate tooth sensitivity and attenuate dental caries infections was published in Germany in 1846 and many times since and that SDF had its start a half century ago in Japan, it is quite puzzling that only now are North American dentists enthusiastically catching on to chemical means of managing dental caries infections. In this case, the old enigmatic question posed by inventors and innovators: "How many years does it take to have an overnight success?" is more appropriately phrased, "How many decades?"
Queries regarding this course may be submitted to authorqueries@aegiscomm.com
Acknowledgments
The authors gratefully acknowledge Leah M. Morano for her thoughtful English translation of the 1846 Zahnarzt article and Nabil Ouatik, DMD, for his assistance in locating the piece in the German dental literature and his thoughts about the translation. The authors would also like to thank the American Academy of the History of Dentistry for graciously permitting them to use text for this article that was adapted from: Croll TP, Berg JH. Silver diammine fluoride: rejuvenation of a 172-year-old (or older?) dental caries attenuation. J Hist Dent. 2018;66(2):54-61.
References
1. Silver. Chemistry Explained website. http://www.chemistryexplained.com/elements/P-T/Silver.html. Accessed September 2, 2020.
2. Lansdown A. Silver in health care: antimicrobial effects and safety in use. Curr Probl Dermatol. 2006;33:17-34.
3. Silver in medicine - past, present, and future. The Silver Institute website. https://www.silverinstitute.org/wp-content/uploads/2017/01/SilverInMedicine.pdf. Accessed September 2, 2020.
4. Alexander, JW. History of the medical use of silver. Surg Infect (Larchmt). 2009;10(3):289-292.
5. Bjørklund, G. [The history of dental amalgam] Tidsskr Nor Laegeforen. 1989;109(34-36):3582-3585.
6. Czarnetzki A, Ehrhardt S. Re-dating the Chinese amalgam-filling of teeth in Europe. International Journal of Anthropology. 1990;5(4):325-332.
7. McCabe JF, Walls AWG. Applied Dental Materials. 9th ed. Oxford, UK: Blackwell Publishing Ltd.; 2008.
8. Soler JI, Ellacuria J, Triana R, et al. A history of dental amalgam. J Hist Dent. 2002;50(3):109-116.
9. Rathore M, Singh A, Pant VA. The dental amalgam toxicity fear: a myth or actuality. Toxicol Int. 2012;19(2):81-88.
10. Condie DF. A Practical Treatise on the Diseases of Children. Philadelphia, PA: Blanchard and Lea; 1847:151.
11. Harris CA. The Principles and Practice of Dental Surgery. 4th ed. Philadelphia, PA: Lindsay & Blakiston;1850:444.
12. Miszellen. Hollenstein bei sehr ausgehohlten Zahnen. Zahnarzt. Berlin, Germany: Verlag von Albert Forstner; 1846:375.
13. Prinz P. Dental Materia Medica and Therapeutics. 4th ed. St. Louis, MO: C.V. Mosby Company; 1916: 217-230.
14. Miller WD. The micro-organisms of the human mouth - the local and general diseases which are caused by them. Philadelphia, PA: The S. S. White Dental Mfg. Co.;1890.
15. Pedley RD. The Diseases of Children's Teeth; Their Prevention And Treatment. London: TP Segg & Co.; 1895:189-190, 196, 209, 219-220, 231, 258.
16. Howe PR. A method of sterilizing and at the same time impregnating with a metal, affected dentinal tissue. Dental Cosmos. 1917;59(9):891-904.
17. Duffin SR. Medical chemotherapeutics. In: Duffin S, Juhl J, Schwab J, Duffin M, ed. SMART Oral Health: The Medical Management of Caries. San Bernadino, CA: Oral Health Outreach, LLC; 2019:13-15.
18. Black GV. Management of children's teeth. In: A Work on Operative Dentistry in Two Volumes Vol. 1, Pathology of the Hard Tissues of the Teeth. 2nd ed. Chicago, Illinois: Medico-Dental Publishing Co.; 1916:230-233, 248-254.
19. Black GV. Treatment of decays of the deciduous incisors and canines. In: A Work on Operative Dentistry in Two Volumes Vol. 1. Pathology of the Hard Tissues of the Teeth. 6th ed. (with revision by Arthur D. Black). Chicago, Illinois: Medico-Dental Publishing Co.; 1924:247-253.
20. Hogeboom FE. Filling materials used in deciduous teeth. In: Practical Pedodontia or Juvenile Operative Dentistry and Public Health Dentistry. St. Louis, MO: C.V. Mosby Company; 1924:60-61.
21. McBride WC. Silver nitrate precipitation. In: Juvenile Dentistry. 2nd ed. London: Henry Kimpton; 1937:192-195.
22. Muhler JC, Hine MK. Operative treatment as a method of dental caries control. In: A Symposium on Preventive Dentistry: With Specific Emphasis on Dental Caries and Periodontial Diseases. St. Louis, MO: C.V. Mosby Company; 1956:161.
23. Lo EC, Duangthip D. Non-restorative approaches for managing cavitated dentin carious lesions: silver fluoride. In: Coelho S, Takeshita EM. eds. Pediatric Restorative Dentistry. Switzerland: Springer Nature; 2019:143.
24. Nishino M. Studies on the topical application of ammoniacal silver fluoride for the arrest of dental caries [in Japanese]. Osaka Daigaku Shigaku Zasshi. 1969;14(1):1-14.
25. Yamaga R, Nishino M, Yoshida S, Yokomizo I. Diammine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972;12:1-20.
26. Tsutsumi N. Studies on topical application of Ag(NH3)2F for the control of interproximal caries in human primary molars: 3. Clinical trial of Ag(NH3)2F on interproximal caries in human primary molars. Jpn J Pediatr Dent. 1981;19(3):537-545.
27. Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81(11):767-770.
28. Llodra JC, Rodriguez A, Ferrer B, et al. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84(8):721-724.
29. Braga MM, Mendes FM, De Benedetto MS, et al. Effect of silver diammine fluoride on incipient caries lesions in erupting permanent first molars: a pilot study. J Dent Child (Chic). 2009;76(1):28-33.
30. Peng JJ, Botelho MG, Matinlinna JP. Silver compounds used in dentistry for caries management: a review. J Dent. 2012;40(7):531-541.
31. Liu BY, Lo EC, Li CM. Effect of silver and fluoride ions on enamel demineralization: a quantitative study using micro-computed tomography. Aust Dent J. 2012;57(1):65-70.
32. Mattos-Silveira J, Floriano I, Ferreira FR, et al. New proposal of silver diamine fluoride use in arresting approximal caries: study protocol for a randomized controlled trial. Trials. 2014;15:448.
33. US Food & Drug Administration. 510(k) Premarket Notification. FDA website. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K102973. Updated August 31, 2020. Accessed September 2, 2020.
34. Clinicians Report Foundation. 38% silver diamine fluoride (SDF): does it arrest dental caries lesion progression? Clinicians Report. 2018;11(1):1-3.
35. Croll TP, Berg JH. Delivery of fluoride solutions to proximal tooth surfaces: Part II: Caries interception with silver diamine fluoride. Inside Dentistry. 2017;13(9):56-58.
36. Croll TP, Berg JH. Silver Diammine fluoride abatement of dental caries infection in primary teeth. Inside Dental Hygiene. 2018;14(9):10-18.
37. Christensen R. Focus On: Silver diamine fluoride. Dentistry Today. 2017;36(2):18.
38. Croll TP, Berg JH. Delivery methods of silver diammine fluoride to contacting proximal tooth surfaces and history of silver in dentistry. Compend Cont Ed Dent. 2020; 41(2):84-90.
39. Clinicians Report Foundation. The epidemic of cervical caries in Class II resin box forms. Clinicians Report. 2018;11(6).
40. Liu BY, Lo EC, Li CM. Effect of silver and fluoride ions on enamel demineralization: a quantitative study using micro-computed tomography. Aust Dent J. 2012;57(1):65-70.
41. Horst JA, Ellenikiotis H, Milgrom PM. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016;44(1):16-28.
42. Mei ML, Lo EC, Chu CH. Clinical use of silver diamine fluoride in dental treatment. Compend Contin Educ Dent. 2016;37(2):93-98.
43. Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016;1(3):201-210.
44. Crystal YO, Niederman RN: Silver diamine fluoride treatment considerations in children's caries management. Pediatr Dent. 2016; 38(7):466-471.
45.Crystal YO, Marghalani AA, Ureles SD, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39(5):135-145.
46.Chibinski AC, Wambier LM, Feltrin J, et al. Silver diamine fluoride has efficacy in controlling caries progression in primary teeth: a systematic review and meta-analysis. Caries Res. 2017;51(5):527-541.
47. Nguyen YHT, Ueno M, Zaitsu T, et al. Caries arresting effect of silver diamine fluoride in Vietnamese preschool children. Int J Clin Prev Dent. 2017;13(3):147-154.
48. Milgrom P, Horst JA, Ludwig S, et al. Topical silver diamine fluoride for dental caries arrest in preschool children: a randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J Dent. 2018;68:72-78.
49. Horst JA. Silver fluoride as a treatment for dental caries. Adv Dent Res. 2018;29(1):135-140.
50. Zhao IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2018;68(2):67-76.
51. Crystal YO, Niederman R. Evidence-based dentistry update on silver diamine fluoride. Dent Clin North Am. 2019;63(1):45-68.
52. Horst JA, Heima M. Prevention of dental caries by silver diamine fluoride. Compend Contin Educ Dent. 2019;40(3):158-163.
53. Young DA, Wong A. Glass ionomer cement as a chemical treatment for caries. In: Duffin S, Juhl J, Schwab J, Duffin M eds. SMART Oral Health: The Medical Management of Caries. San Bernadino, CA: Oral Health Outreach, LL.; 2019:69-77.
54. Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: A comprehensive overview. Clin Oral Investig. 2012;16(5):1337-1346.
55. Callister C, Callister M, Nolan M, et al. Preventative agents: The multiple uses of silver nanoparticles in dentistry. Compend Contin Educ Dent. 2020;41(3):143-147.