You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Arriving at the most accurate clinical diagnosis is the goal of every dentist in every clinical situation for every patient. Unfortunately, it is still common for dentists today to use phrases in their case presentations such as, "it could be," "you may have," "I'm not sure," or "we could try." This uncertainty is often a result of their reliance on 2D radiography, which presents complex, layered, 3D information in a 2D format. Too much information is compressed into a single periapical or panoramic radiograph to be fully understood. Oftentimes, this distortion of information leads to misinterpretation during diagnosis, and it can even lead to a clinician missing certain findings entirely. Furthermore, when patients are brought into the discussion, they have an even harder time understanding the information that defines their diagnoses because they have not been trained to interpret radiographs. This limited understanding can affect their willingness to participate in the treatment presented. Treatment plans may vary from dentist to dentist, but all clinical diagnoses should be consistent and accurate to the level that our technology and experience allows.
Three-dimensional imaging utilizing cone-beam computed tomography (CBCT) is available to today's dental practices, and it has the potential to make dentists into better diagnosticians as well as to help them better educate their patients. Its use can also result in the creation of more appropriate treatment plans and encourage patients to become more involved in understanding and choosing from potential options. CBCT systems, which are variations of traditional medical CT systems, have been used in dentistry since the early 2000s. The unit rotates around the patient and captures data using a cone-shaped X-ray beam. That information is then reconstructed into a 3D image of the dentition, oral and maxillofacial region, ears, nose, and throat.1 Regarding the hard tissues and teeth, CBCT offers higher resolution and image sharpness when compared with medical CT.2
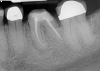
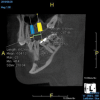
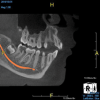
The idea that a dentist may be incorrect in his or her diagnosis is distasteful, but a reality that this profession wrestles with on a daily basis. An image comparison can help to clarify this thought. The first image is a 2D radiograph of tooth No. 19 that includes the buccal cortical plate the lingual cortical plate and approximately 10 mm of trabecular bone compressed into a single image (Figure 1). Because the full width and volume of the tooth is included in the image, any existing pathoses could be masked or hidden in a fog of digital information. A CBCT scan of the same tooth provides more detail because it can present a slice (0.1 mm) of information from the center of the area in question (Figure 2). All of the extraneous information is eliminated, and the clinician and the patient have a more precise picture to evaluate. Furthermore, a periapical radiograph can be distorted by the angle of the cone to the sensor, whereas a CBCT scan has no distortion and is accurate in all views. With a CBCT scan, the clinician is able to state with certainty that a condition exists, and the patient is able to more clearly understand what his or her condition is when considering the available choices for treatment.
Comparative Radiation Exposure
Some clinicians object to the use of CBCT, citing concerns regarding the amount of ionizing radiation that patients are exposed to from a CBCT scan when compared with a panoramic radiograph or a full mouth series of radiographs; however, these points of view usually stem from a lack of experience or a lack of knowledge about the current state of CBCT technology. Although the effective radiation doses of intraoral radiographs (< 1.5 µSv), panoramic radiographs (2.7 µSv to 24.3 µSv), and cephalometric radiographs (< 6 µSv) are typically lower3 than those required by CBCT units, which range from 19 µSv to 1,073 µSv,4-6 the effective radiation dose of CBCT is significantly less than that of multislice CT, which ranges from 280 µSv to 1,410 µSv,3,6 and the effective dose required for a full mouth series of radiographs can total as much as 170 µSv.7
One modern CBCT machine, for example, exposes patients to approximately 78 µSv for a standard adult scan (8 cm x 10 cm FOV). A full mouth series could exceed this exposure by as much as 92 µSv, and that's if the clinician doesn't have to do any retakes, otherwise, it could be more. A panoramic radiograph produces less radiation than the CBCT scan, but it is hampered by distortion (30% to 40% or more) and magnification issues that result in a lack of clarity for single tooth issues. Moreover, a panoramic radiograph and 4 common bitewing radiographs can add up to as much as 30 µSv or more. The amount of radiation exposure from modern CBCT is very low comparatively; however, it is still dependent on the field of view chosen and the speed of exposure. For example, a pediatric rapid scan is associated with approximately 25 µSv of exposure. This is roughly equivalent to many panoramic radiographs, but the images encompass the entire mouth and provide volume and clarity that exceed the diagnostic information that can be obtained from a panoramic radiograph.
Historically, dentistry has done an excellent job of reducing the amount of radiation exposure as digital technology has improved.8,9 A current CBCT scan exposure involves far less radiation than traditional film exposures, and the amount can be seen as clinically insignificant when compared with the amounts associated with other routinely taken images, such as medical CT scans, which can expose patients to radiation doses ranging from 1,000 µSv to 30,000 µSv.10 Furthermore, many CBCT units utilize larger focal spots in the range of 0.5 mm to 0.7 mm to reduce radiation,11 and some offer reconstruction times as fast as 30 seconds.11 Lower-dose CBCT scans expose patients to less radiation than they would receive during a cross-country airplane flight.12
Clinical Applications of CBCT
Another objection to CBCT that is voiced by the profession is that it has limited clinical applications. Is a CBCT scan only appropriate when providing implants? The answer is emphatically no. The applications of CBCT include pediatric dentistry, orthodontics, endodontics, periodontics, restorative dentistry, implant dentistry, oral surgery, and temporomandibular joint (TMJ) therapy.8 There is even an emerging area of interest in dentistry involving the evaluation and treatment of airway issues that requires 3D imaging.13 It could be argued that this technology should be a part of any complete diagnosis on every patient.
Pediatric Dentistry
Taking a CBCT scan of a child can present a variety of advantages. It is extraoral, which encourages cooperation, and it provides a view of the entire mouth. Although clinicians may initially be looking for caries, they can also see developing dentitions and eruption patterns. This permits early interceptive orthodontic care when indicated or airway management combined with orthodontic care when appropriate for a developing child. The ability to visualize the presence or absence of the permanent dentition as well as the specific anatomy and positions of the teeth prior to eruption is educational for the dentist and the parents and allows for the best preparation for and timing of any needed treatment (Figure 3).
Orthodontics
Similar to the use of CBCT in pediatric dentistry, the ability to visualize that the dentition is developing properly is invaluable at all ages. Understanding the angulation and rotation of the teeth prepares clinicians for the mechanics necessary to treat each individual case. In addition, for adult orthodontics, having a measurable view of the bone thickness and structures around the roots of the permanent dentition is key to the successful treatment of a mouth that is not dynamically growing or changing. This can help the clinician to avoid moving roots out of their bony housings and, possibly, to reduce the blunting of roots and other potential mishaps involving tooth movement. Many newer CBCT units have an optional cephalometric attachment available for orthodontic evaluation.
Endodontics
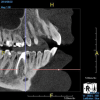
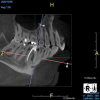
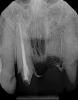
Being able to see the number and shape of the canals accurately prior to treatment is the desire of any clinician who performs endodontics. Research suggests that, due to improved diagnostic accuracy, the final treatment plan may change in up to 50% of endodontic cases if CBCT is used rather than traditional 2D imaging.14,15 The question of whether or not a patient has an MB2 canal can be answered prior to opening the access preparation (Figure 4 and Figure 5). Visualizing single canals that bifurcate in the apical or middle third of the root or those that merge to a single apical opening can help clinicians to understand their instrumentation needs in advance. In addition, the ability to measure the length and shape of a canal planned for instrumentation prior to utilizing an apex locator helps to confirm any measurements obtained by other means. It should also be noted that the ability to see a pathosis in 3 dimensions and to involve the patient in understanding his or her condition prior to any decision-making allows for definitive treatment planning. In fact, many patients have pathoses associated with teeth that are asymptomatic that remain unknown to them until they are visually presented with the evidence (Figure 6).
Periodontics
With CBCT, the topography of the bone around every root is visible. Any loss of bone between teeth, including furcation involvements and lingual pockets, that is not visible on 2D radiographs can be fully visualized, and when combined with the soft-tissue measurements provided, clinicians and patients are equipped with a clear map of the existing condition. This can aid in site-specific treatment planning and predicting likely outcomes and has also been shown to help educate patients and motivate them to practice better hygiene habits.
Restorative Dentistry
Being able to see the location and depth of caries, the presence of cracks in teeth and roots, and other oral pathoses that may or may not be present aids clinicians in both treatment planning and patient education. When caries is located very near a pulp chamber, but no pathosis is present at the apex of the root and the tooth tests vital, the clinician can be more optimistic about restoring the tooth without the need for endodontic therapy or extraction. However, if a pathosis is present on the CBCT scan, then the patient, who may or may not exhibit symptoms, can make an informed decision regarding whether to undergo endodontic therapy or remove the tooth. When CBCT is employed in diagnosis, clinicians find that guessing about the condition of a tooth is replaced with knowing the condition. Communication with patients is enhanced, as is their understanding, and the most appropriate treatment plans can be created.
Implant Dentistry
The use of CBCT has been shown to reduce the rate of implant failures.8 Placing a root-form implant into an asymmetrical section of bone can be done more accurately and safely if the location is visualized in 3D prior to placement. The primary advantage of a cross-sectional or coronal view of the bone is that it shows the shape of the anatomy, and any measurements taken from a CBCT image are accurate to 0.1 mm. The placement of an implant to replace a single tooth is far easier to accomplish when the adjacent roots and other important nearby structures, such as the inferior alveolar nerve and the sinus, are identified and measured relative to the desired position of the implant. In addition, CBCT enables an implant to be virtually placed prior to the actual surgery.16 The need for an accurate digital map only increases if a case involves multiple implants or is otherwise more complex (Figure 7). Regardless of the complexity, many clinicians who place implants advocate for the use of surgical guides to aid in precise positioning. This is another important use of CBCT in implant dentistry. Accurate surgical guide fabrication requires a clear and accurate CBCT digital imaging and communications in medicine (DICOM) file to be sent to the party constructing the guide.17
Oral Surgery
Identifying the shape and location of the roots of teeth to be removed is critical to performing safe exodontia. Some clinicians virtually deconstruct teeth using CBCT images prior to actually sectioning and removing them. Being able to recognize pathoses and differentiate affected structures from normal structures is key in deciding what the treatment should be and when that treatment should be initiated (Figure 8 through Figure 10). The arena of the oral surgeon is larger than that of many general practitioners, involving the sinuses and condyles and other considerations in and around the entire mandible and maxilla. Certain fractures and other conditions that some general practitioners feel uncomfortable treating are often referred for evaluation and treatment by an oral surgeon. Because of this, oral surgeons require the most accurate and complete diagnostic information available. The American Academy of Oral and Maxillofacial Radiology recommends that "cross-sectional imaging be used for the assessment of all dental implant sites" and has stated that "CBCT is the imaging method of choice for gaining this information."18
TMJ Therapy
Although there are many different approaches to managing problems associated with musculoskeletal dysfunction of the mandible, any clinician who is involved in providing a diagnosis or any form of treatment would benefit from a CBCT image of the condyles in 3 dimensions. This can be obtained in a closed-bite or open-bite manner and with or without an appliance in the mouth. Assessing the condyles' shape and position relative to the fossa and eminence can be particularly helpful in determining the correct course of treatment for a patient.
Airway Management
This relatively new and evolving area of dentistry, which involves screening for and partnering with physicians to treat issues associated with patients' airways, utilizes CBCT images to observe the size and shape of the airway in combination with other diagnostic tests to identify problems and help determine the best method of treatment. The functionality of the CBCT images in this process is still being evaluated and modified as this area of treatment continues to grow and develop.9,13 However, the ability to determine the airway area can be critical in some cases because an airway size of less than 52 mm2 is associated with a high probability of severe obstructive sleep apnea, and an airway size of 52 mm2 to 110 mm2 is associated with an intermediate probability.19
Training and Scope
Are most or all dentists qualified to read CBCT images? Although the technology can be intimidating to clinicians who are not experienced in its use, the truth of the matter is that it is easier to identify structures and pathoses in CBCT images than in any 2D radiograph. This is made clear by the ability of patients to see and understand the images presented to them without receiving any formal training whatsoever. Because all dentists are trained in radiology, they can easily read a radiographic image created by a cone beam. The real issue for clinicians involves mastery of the software that their particular CBCT unit uses so that they can manipulate the images and best visualize the area in question.9 To this end, the education and training provided by the manufacturers of CBCT units can be very helpful to clinicians before they are able to gain experience through multiple evaluations of images (Figure 11 and Figure 12).
Because CBCT scans provide so much information, some clinicians question the limits of what they are responsible for diagnosing. That is the wrong question to be asking. All dentists are responsible for the diagnosis of any condition in the oral cavity. The correct question that these clinicians need to be asking is what exactly are they missing on their 2D radiographs that they are unaware of but just as responsible for? With CBCT, the clinician misses less, diagnoses more accurately, and can present all of the conditions to the patient instead of just addressing his or her chief complaint. In situations where a CBCT scan is acquired and no pathosis is noted, when the clinician pronounces the patient healthy, he or she will be more accurate in that diagnosis as well.
Dentists who become experienced in evaluating CBCT images become more advanced in their knowledge of anatomy as well as their familiarity with variations in normal structures. As they experience more findings, they also learn to better differentiate between normal and pathological scenarios and recognize pathoses in greater depth and detail. If dentists see something that they are not familiar with or comfortable identifying, they can refer the patient to an oral and maxillofacial radiologist.
Conclusion
In conclusion, one of the most important aspects of any dental practice is the requirement to render an accurate diagnosis for every patient examined. The CBCT technologies available today provide clinicians with the very best information to help them make accurate diagnoses. CBCT is applicable to all aspects of the general dental practice. It benefits dentists by reducing the chances of overlooking problems, reducing the potential for misdiagnosis, and encouraging the development of more appropriate treatment plans, and it benefits patients by providing them with clear images of their conditions that are easy to understand. The concept of evolving from traditional protocols involving 2D radiography to ones involving 3D CBCT is difficult to embrace for some clinicians but necessary for those who wish to grow in the profession and improve the quality of their patients' care.
Queries regarding this course may be submitted to authorqueries@aegiscomm.com
About the Author
Jon Julian, DDS
Private Practice
Travelers Rest, South Carolina
References
1. U.S. Food & Drug Administration. Dental cone-beam computed tomography. FDA website. https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/dental-cone-beam-computed-tomography. Updated September 28, 2020. Accessed May 18, 2021.
2. von See C, Bormann KH, Schumann P, et al. Forensic imaging of projectiles using cone-beam computed tomography. Forensic Sci Int. 2009;190(1-3):38-41.
3. Suomalainen A, Esmaeili EP, Robinson S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging. 2015;6(1):1-16.
4. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(1):106-114.
5. Pauwels R, Beinsberger J, Collaert B, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012;81(2):267-271.
6. Li Gang. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci Dent. 2013;43(2):63-69.
7. American Dental Association. Oral health topics: X-Rays/radiographs. ADA website. https://www.ada.org/en/member-center/oral-health-topics/x-rays. Updated August 13, 2019. Accessed May 18, 2021.
8. Alamri HM, Sadrameli M, Alshalhoob MA, et al. Applications of CBCT in dental practice: a review of the literature. Gen Dent. 2012;60(5):390-400.
9. Pauwels R, Araki K, Siewerdsen, JH, Thonvigitmance SS. Technical aspects of dental CBCT: state of the art. Dentomaxillofac Radiol. 2015;44(1):20140224.
10. Harvard Health Publishing. Radiation risk from medical imaging. Harvard Medical School website. https://www.health.harvard.edu/
cancer/radiation-risk-from-medical-imaging. Published, January 29, 2020. Accessed May 18, 2021.
11. Nemtoi A, Czink C, Haba D, Gahleitner A. Cone beam CT: a current overview of devices. Dentomaxillofac Radiol. 2013;42(8):20120443.
12. Friedberg W, Copeland K, Duke FE, et al. Radiation exposure during air travel: guidance provided by the Federal Aviation Administration for air carrier crews. Health Phys. 2000;79(5):591-595.
13. Lenza MG, de O. Lenza MM, Dalstra M et al. An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res. 2010;13(2):96-105.
14. Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014;40(7):910-916.
15. Mota de Almeida FJ, Knutsson K, Flygare L. The impact of cone beam computed tomography on the choice of endodontic diagnosis. Int Endod J. 2015;48(6):564-572.
16. Fokas G, Vaughn VM, Scarfe WC, Bornstein MM. Accuracy of linear measurements on CBCT images related to pre-surgical implant treatment planning: a systematic review. Clin Oral Implants Res. 2018;29(Suppl 16):393-415.
17. Chan HL, Misch K, Wang HL. Dental imaging in implant treatment planning. Implant Dent. 2010;19(4):288-298.
18. Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):817-826.
19. Hatcher DC. Cone beam computed tomography: craniofacial and airway analysis. Dent Clin North Am. 2012;56(2):343-357.